Nursing Paper Example on Ankylosing Spondylitis: A Comprehensive Overview
/in Assignment Help, Assignment Help Nursing, BLOG, Homework Help, Nursing Exam Help, Nursing Paper Help, Solved Nursing Essays /by Aimee GraceNursing Paper Example on Ankylosing Spondylitis: A Comprehensive Overview
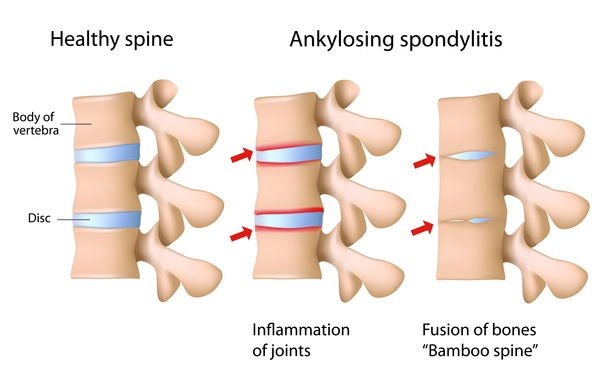
Ankylosing spondylitis (AS) is a chronic inflammatory condition that primarily affects the spine and sacroiliac joints, belonging to the broader category of spondyloarthritis. It is characterized by persistent low back pain and stiffness, typically beginning in early adulthood and disproportionately affecting men. While the exact cause of AS remains elusive, a combination of genetic predisposition, particularly the presence of the human leukocyte antigen (HLA)-B27 gene, and environmental factors is believed to contribute to its development. The inflammation associated with AS can lead to structural damage and fusion of the spine, resulting in significant disability and reduced quality of life for affected individuals. Early recognition and management of AS are crucial to alleviate symptoms, preserve joint function, and improve long-term outcomes. This paper aims to explore the causes, signs and symptoms, etiology, pathophysiology, diagnostic criteria, treatment regimens, patient education, and conclusion regarding ankylosing spondylitis. (Nursing Paper Example on Ankylosing Spondylitis: A Comprehensive Overview)
Causes
The precise cause of ankylosing spondylitis (AS) remains elusive, yet a combination of genetic and environmental factors is believed to contribute to its onset. Among the genetic factors, the human leukocyte antigen (HLA)-B27 gene has a profound association with AS, as it is present in over 90% of individuals with the condition. The HLA-B27 gene plays a crucial role in the immune system’s function, and its presence in AS patients suggests an autoimmune component to the disease.
Environmental factors also play a significant role in triggering AS in genetically susceptible individuals. Bacterial infections, particularly those affecting the gastrointestinal tract, have been implicated as potential environmental triggers. It is hypothesized that bacterial antigens may cross-react with HLA-B27, leading to an aberrant immune response and chronic inflammation in susceptible individuals.
Furthermore, lifestyle factors such as smoking have been identified as potential risk factors for AS. Smoking not only increases the risk of developing AS but also exacerbates disease severity and progression. The exact mechanism by which smoking contributes to AS pathogenesis is not fully understood, but it is thought to involve its pro-inflammatory effects on the immune system.
Additionally, hormonal factors may play a role in AS susceptibility, as the condition disproportionately affects men compared to women. Some studies suggest that sex hormones, particularly testosterone, may influence the development and progression of AS. However, further research is needed to elucidate the exact mechanisms underlying hormonal influences on AS.
In summary, ankylosing spondylitis is a complex disease with a multifactorial etiology involving genetic predisposition, environmental triggers, lifestyle factors such as smoking, and hormonal influences. Understanding the interplay between these factors is crucial for elucidating the underlying mechanisms of AS and developing targeted interventions for its prevention and treatment. (Nursing Paper Example on Ankylosing Spondylitis: A Comprehensive Overview)
Signs and Symptoms
Ankylosing spondylitis (AS) manifests with a range of signs and symptoms that primarily affect the axial skeleton, including the spine and sacroiliac joints, as well as peripheral joints. The hallmark symptom of AS is chronic low back pain and stiffness, which typically begins insidiously and worsens over time. The pain is often worse in the morning or after periods of inactivity and improves with movement and exercise. Additionally, individuals with AS may experience pain and stiffness in other joints, such as the hips, shoulders, and knees, which can significantly impact daily activities and mobility.

Another common symptom of AS is fatigue, which can be debilitating and affect various aspects of daily life, including work, social activities, and leisure pursuits. Fatigue in AS is often multifactorial, resulting from a combination of chronic pain, inflammation, poor sleep quality, and psychological factors such as stress and depression.
In severe cases, ankylosing spondylitis can lead to spinal deformities and impaired mobility. As the disease progresses, chronic inflammation of the spinal vertebrae can cause them to fuse together, resulting in a rigid, stooped posture known as kyphosis. This can lead to limitations in spinal mobility, making it difficult for individuals with AS to perform activities of daily living and participate in physical activities.
Other less common symptoms of AS may include inflammation of the eyes (uveitis), inflammatory bowel disease (such as Crohn’s disease or ulcerative colitis), and cardiovascular complications (such as aortitis or conduction abnormalities). These extra-articular manifestations can vary in severity and may require specialized treatment and management in addition to addressing the underlying AS symptoms.
Overall, recognizing the signs and symptoms of ankylosing spondylitis is crucial for early diagnosis and initiation of appropriate treatment to help alleviate pain, improve mobility, and enhance quality of life for affected individuals. (Nursing Paper Example on Ankylosing Spondylitis: A Comprehensive Overview)
Etiology
Ankylosing spondylitis (AS) is a complex disease with a multifaceted etiology involving genetic, environmental, and immunological factors. The strongest genetic association with AS is the presence of the human leukocyte antigen (HLA)-B27 gene, which is found in over 90% of individuals with the condition. HLA-B27 is a major histocompatibility complex (MHC) class I molecule that plays a crucial role in the immune system’s ability to recognize and respond to foreign antigens. Although the exact mechanism by which HLA-B27 contributes to AS pathogenesis remains unclear, it is thought to involve aberrant immune responses to self-antigens, leading to chronic inflammation and tissue damage in susceptible individuals.
Environmental factors also play a significant role in AS development, particularly in triggering disease onset in genetically predisposed individuals. Bacterial infections, particularly those affecting the gastrointestinal tract, have been implicated as potential environmental triggers for AS. It is hypothesized that bacterial antigens may cross-react with HLA-B27, triggering an exaggerated immune response and chronic inflammation in susceptible individuals.
Furthermore, lifestyle factors such as smoking have been identified as potential risk factors for AS. Smoking not only increases the risk of developing AS but also exacerbates disease severity and progression. The exact mechanism by which smoking contributes to AS pathogenesis is not fully understood, but it is thought to involve its pro-inflammatory effects on the immune system.
Overall, the etiology of ankylosing spondylitis is complex and multifactorial, involving a combination of genetic predisposition, environmental triggers, and immunological dysregulation. Understanding the interplay between these factors is crucial for elucidating the underlying mechanisms of AS and developing targeted interventions for its prevention and treatment. (Nursing Paper Example on Ankylosing Spondylitis: A Comprehensive Overview)
Pathophysiology
The pathophysiology of ankylosing spondylitis (AS) revolves around chronic inflammation of the axial skeleton, primarily affecting the sacroiliac joints and the spine. The initial trigger for the inflammatory process in AS is not fully understood, but it is believed to involve a combination of genetic predisposition, environmental factors, and immune dysregulation.
In genetically susceptible individuals, such as those carrying the human leukocyte antigen (HLA)-B27 gene, environmental triggers such as bacterial infections may activate the immune system. This results in an exaggerated inflammatory response characterized by the infiltration of immune cells, particularly T lymphocytes, into the affected joints.
The inflammatory process in AS primarily targets the entheses, which are the sites where ligaments and tendons attach to bone. Chronic inflammation at the entheses leads to fibrocartilage proliferation, bone erosion, and eventual new bone formation, a process known as syndesmophyte formation. This process contributes to the characteristic radiographic findings of AS, including sacroiliitis, vertebral squaring, and syndesmophytes.
Furthermore, the inflammatory cytokines released during the inflammatory process, such as tumor necrosis factor-alpha (TNF-α) and interleukin-17 (IL-17), play a crucial role in perpetuating the inflammatory cascade and tissue damage in AS. These cytokines promote the recruitment and activation of immune cells, as well as the production of matrix metalloproteinases (MMPs), which contribute to joint destruction and remodeling.
Over time, chronic inflammation and tissue damage in AS can lead to spinal fusion and structural deformities, resulting in reduced spinal mobility and impaired quality of life for affected individuals. Understanding the underlying pathophysiology of AS is essential for developing targeted therapies aimed at mitigating inflammation, preserving joint function, and improving long-term outcomes for patients with this chronic inflammatory condition. (Nursing Paper Example on Ankylosing Spondylitis: A Comprehensive Overview)
DMS-5 Diagnosis
Diagnosing ankylosing spondylitis (AS) typically involves a comprehensive evaluation based on clinical presentation, imaging studies, and laboratory tests. According to the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), the criteria for diagnosing AS include:
- Evidence of Sacroiliitis: Imaging studies such as X-rays or magnetic resonance imaging (MRI) showing evidence of sacroiliitis, which is inflammation of the sacroiliac joints. Sacroiliitis is a hallmark feature of AS and is characterized by joint erosions, sclerosis, and joint space narrowing.
- Chronic Low Back Pain: Persistent low back pain and stiffness lasting for at least three months, which typically improves with exercise and worsens with rest. The pain is often insidious in onset and may be accompanied by morning stiffness, which improves with physical activity.
- Limitation of Spinal Mobility: Decreased spinal mobility in both the sagittal and frontal planes, as assessed by clinical examination. Patients with AS may have difficulty bending forward, backward, or to the sides due to inflammation and structural changes in the spine.
- Extra-articular Manifestations: Presence of extra-articular manifestations commonly associated with AS, such as uveitis (inflammation of the eye), inflammatory bowel disease (such as Crohn’s disease or ulcerative colitis), and cardiovascular complications (such as aortitis or conduction abnormalities).
- Laboratory Findings: Although not specific for AS, laboratory tests such as erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) may be elevated, indicating the presence of systemic inflammation.
By meeting these criteria, along with a thorough clinical assessment and exclusion of other potential causes of back pain, healthcare providers can confidently diagnose ankylosing spondylitis according to DSM-5 guidelines. (Nursing Paper Example on Ankylosing Spondylitis: A Comprehensive Overview)
Treatment Regimens and Patient Education
Treatment for ankylosing spondylitis (AS) aims to alleviate symptoms, reduce inflammation, preserve joint function, and improve overall quality of life. Management of AS typically involves a multimodal approach that includes pharmacological interventions, physical therapy, exercise, patient education, and lifestyle modifications.
Pharmacological Interventions: Nonsteroidal anti-inflammatory drugs (NSAIDs) are often the first-line treatment for managing pain and inflammation in AS. NSAIDs can help relieve symptoms and improve mobility by reducing inflammation in affected joints. In cases where NSAIDs are ineffective or poorly tolerated, disease-modifying antirheumatic drugs (DMARDs) such as sulfasalazine or methotrexate may be prescribed to suppress the underlying inflammatory process. Biologic agents, such as tumor necrosis factor-alpha (TNF-α) inhibitors or interleukin-17 (IL-17) inhibitors, are reserved for patients with moderate to severe AS who do not respond adequately to conventional treatments.
Physical Therapy and Exercise: Physical therapy plays a crucial role in AS management by improving joint flexibility, strength, and posture. A tailored exercise program, including stretching, strengthening, and aerobic exercises, can help reduce pain, improve mobility, and prevent spinal deformities. Patients should be encouraged to engage in regular physical activity to maintain joint function and overall physical health.
Patient Education: Patient education is essential in empowering individuals with AS to actively participate in their treatment and self-care. Patients should be educated about the chronic nature of AS and the importance of adhering to their treatment regimens. They should also be informed about strategies for managing pain and stiffness, such as proper posture, ergonomic modifications, and the use of heat or cold therapy. Additionally, patients should be educated about the potential complications of AS, including spinal deformities, cardiovascular complications, and extra-articular manifestations, and the importance of regular monitoring and follow-up with healthcare providers.
Lifestyle Modifications: Lifestyle modifications can also play a significant role in managing AS symptoms and improving overall quality of life. Patients should be encouraged to maintain a healthy weight, avoid smoking, and minimize alcohol consumption, as these factors can exacerbate inflammation and disease progression. Additionally, patients should be educated about ergonomic principles and proper body mechanics to prevent joint strain and injury.
A comprehensive treatment approach for ankylosing spondylitis involves a combination of pharmacological interventions, physical therapy, exercise, patient education, and lifestyle modifications. By addressing both the symptoms and underlying inflammatory process, healthcare providers can help improve outcomes and enhance quality of life for individuals with AS. (Nursing Paper Example on Ankylosing Spondylitis: A Comprehensive Overview)
Conclusion
Ankylosing spondylitis (AS) is a complex chronic inflammatory condition that primarily affects the spine and sacroiliac joints, leading to pain, stiffness, and impaired mobility. Through a deeper understanding of its causes, signs and symptoms, etiology, pathophysiology, DSM-5 diagnosis, treatment regimens, and patient education, healthcare providers can offer more effective management strategies for individuals with AS. By emphasizing a multimodal treatment approach that includes pharmacological interventions, physical therapy, exercise, patient education, and lifestyle modifications, healthcare providers can help alleviate symptoms, reduce inflammation, preserve joint function, and improve overall quality of life for patients with AS. Continued research into the underlying mechanisms of AS and the development of targeted therapies will further enhance our ability to manage this chronic inflammatory condition and improve outcomes for affected individuals. (Nursing Paper Example on Ankylosing Spondylitis: A Comprehensive Overview)



