Nursing Paper Example on Bacterial Meningitis: Understanding the Threat
Nursing Paper Example on Bacterial Meningitis: Understanding the Threat
Causes
Bacterial meningitis emerges from a confluence of factors, primarily orchestrated by a group of nefarious bacteria adept at infiltrating the body’s defenses. Among the most notorious perpetrators are Neisseria meningitidis, Streptococcus pneumoniae, and Haemophilus influenzae type b. These microbial miscreants gain entry into the bloodstream through various portals, including respiratory droplets expelled during coughing or sneezing, direct contact with contaminated surfaces, or intimate contact with an infected individual.
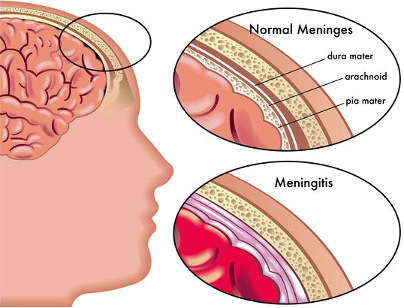
Once in the bloodstream, these bacterial invaders embark on a treacherous journey, traversing the circulatory system with stealthy precision until they reach their ultimate destination: the brain and spinal cord. Here, they encounter the formidable blood-brain barrier, a fortress-like defense mechanism designed to safeguard the sanctity of the central nervous system. Despite its formidable nature, this barrier proves penetrable to certain bacterial species, allowing them to breach its defenses and initiate their malevolent assault on the meninges—the protective membranes enveloping the brain and spinal cord.
Several predisposing factors can facilitate the insidious entry of these bacteria into the bloodstream. Respiratory infections, such as sinusitis or otitis media, provide convenient portals of entry, allowing bacteria easy access to the bloodstream. Similarly, individuals with compromised immune systems due to underlying medical conditions or immunosuppressive medications are more susceptible to bacterial meningitis.
Moreover, trauma or injury to the skull, such as skull fractures or surgical procedures involving the head or neck, can compromise the integrity of the blood-brain barrier, creating an opportune pathway for bacterial invasion. Additionally, certain lifestyle factors, such as smoking or living in crowded environments, may increase the risk of exposure to bacterial pathogens responsible for meningitis.
In essence, bacterial meningitis is a multifaceted disease driven by the interplay of bacterial pathogens, host susceptibility factors, and environmental influences. Understanding the intricacies of its causative factors is paramount in devising effective preventive strategies and therapeutic interventions to combat this formidable foe. (Nursing Paper Example on Bacterial Meningitis: Understanding the Threat)
Signs and Symptoms
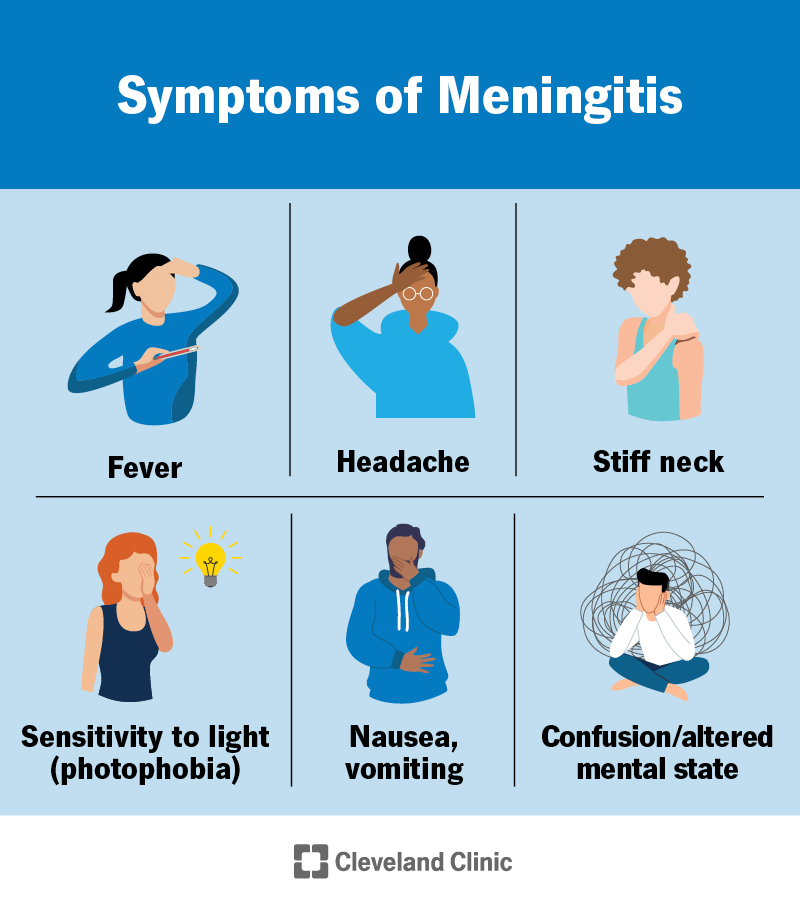
Bacterial meningitis is characterized by a diverse array of signs and symptoms that reflect the profound impact of inflammation on the central nervous system. The clinical presentation of bacterial meningitis can vary widely, depending on factors such as age, immune status, and the specific bacterial pathogen involved.
One of the hallmark features of bacterial meningitis is the sudden onset of symptoms, often accompanied by a rapid progression of illness. Fever is a common early sign, often accompanied by chills and rigors, reflecting the body’s immune response to the invading pathogens. Additionally, individuals may experience a severe headache, described as intense and unrelenting, which may be exacerbated by changes in body position.
A stiff neck, or nuchal rigidity, is another classic symptom of bacterial meningitis, resulting from inflammation of the meninges and irritation of the spinal nerves. This stiffness can make it difficult for individuals to flex their necks forward, a characteristic finding observed during physical examination.
Sensitivity to light, known as photophobia, is another prominent feature of bacterial meningitis, as the inflamed meninges become hypersensitive to external stimuli such as bright lights. This symptom often manifests as discomfort or pain in the eyes when exposed to light.
In addition to these cardinal symptoms, individuals with bacterial meningitis may experience a constellation of neurological manifestations, including confusion, altered mental status, and seizures. In infants and young children, the clinical presentation may be more subtle and nonspecific, with symptoms such as irritability, poor feeding, lethargy, and a bulging fontanelle.
Prompt recognition and evaluation of these signs and symptoms are crucial for early diagnosis and initiation of appropriate treatment. Timely intervention can help prevent serious complications and improve outcomes for individuals affected by bacterial meningitis. (Nursing Paper Example on Bacterial Meningitis: Understanding the Threat)
Etiology
Bacterial meningitis unfolds as a complex interplay between microbial invaders, host vulnerabilities, and environmental factors, culminating in a cascade of events that precipitate inflammation of the meninges—the protective membranes enveloping the brain and spinal cord.
Respiratory infections serve as common precursors to bacterial meningitis, providing a gateway for microbial entry into the bloodstream. Conditions such as sinusitis, otitis media, or pneumonia create conducive environments for bacterial proliferation, facilitating their dissemination to the central nervous system.
Individuals with compromised immune systems are particularly susceptible to bacterial meningitis, as their diminished defenses offer little resistance against invading pathogens. Underlying medical conditions, such as HIV/AIDS, diabetes mellitus, or malignancies, weaken the immune response, rendering individuals more vulnerable to infectious threats.
Trauma or injury to the head or neck region can compromise the integrity of the blood-brain barrier, paving the way for bacterial infiltration into the central nervous system. Skull fractures, penetrating head injuries, or neurosurgical procedures disrupt the protective barriers that normally shield the brain and spinal cord from microbial assault, increasing the risk of bacterial meningitis.
Certain lifestyle factors and environmental influences also contribute to the etiology of bacterial meningitis. Crowded living conditions, such as dormitories or military barracks, facilitate the transmission of respiratory pathogens among individuals in close proximity. Smoking, alcohol abuse, and illicit drug use can impair immune function and respiratory health, exacerbating the risk of bacterial infections.
Overall, bacterial meningitis arises from a complex interplay of microbial, host, and environmental factors. Understanding the multifaceted etiology of this condition is crucial in implementing preventive measures and targeted interventions to mitigate its impact on public health. (Nursing Paper Example on Bacterial Meningitis: Understanding the Threat)
Pathophysiology
The pathophysiology of bacterial meningitis is characterized by a series of intricate events that unfold within the central nervous system, orchestrated by the insidious invasion of pathogenic bacteria and the host’s robust inflammatory response.
Following the breach of the blood-brain barrier by bacterial pathogens, typically originating from a primary infection site such as the respiratory tract or bloodstream, these microbial invaders gain access to the cerebrospinal fluid (CSF) and the meninges—the delicate membranes enveloping the brain and spinal cord.
Once within the CSF and meninges, bacteria unleash a torrent of virulence factors and toxins, triggering a robust immune response characterized by the release of pro-inflammatory cytokines, chemokines, and other mediators of inflammation. These inflammatory mediators recruit immune cells, such as neutrophils and macrophages, to the site of infection, amplifying the inflammatory cascade and contributing to tissue damage.
The inflammatory response within the meninges leads to a constellation of clinical manifestations, including fever, headache, and nuchal rigidity. The release of pro-inflammatory cytokines also disrupts the blood-brain barrier, facilitating the infiltration of immune cells and circulating inflammatory mediators into the brain parenchyma, further exacerbating neuronal injury and tissue damage.
Moreover, the inflammatory cascade induces an increase in intracranial pressure, compromising cerebral blood flow and leading to cerebral edema—a hallmark feature of severe bacterial meningitis. Cerebral edema exacerbates neuronal injury, impairs neurological function, and contributes to the development of life-threatening complications such as seizures, cerebral herniation, and brainstem compression.
In summary, the pathophysiology of bacterial meningitis is characterized by a complex interplay of microbial virulence factors, host immune responses, and inflammatory mediators, culminating in neuronal injury, tissue damage, and the development of severe neurological complications. Understanding these intricate disease processes is crucial in guiding therapeutic interventions and improving outcomes for individuals affected by bacterial meningitis. (Nursing Paper Example on Bacterial Meningitis: Understanding the Threat)
DSM-5 Diagnosis
The diagnosis of bacterial meningitis relies on a combination of clinical assessment, laboratory investigations, and neuroimaging studies, guided by established criteria outlined in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5).
Clinically, individuals with suspected bacterial meningitis typically present with a constellation of symptoms, including fever, headache, nuchal rigidity, and altered mental status. These clinical features raise suspicion for meningitis and warrant further evaluation.
Laboratory investigations play a pivotal role in confirming the diagnosis of bacterial meningitis. Cerebrospinal fluid (CSF) analysis, obtained via lumbar puncture, is a cornerstone diagnostic test. CSF analysis typically reveals an elevated white blood cell count, predominantly consisting of neutrophils, indicative of an inflammatory response. Additionally, CSF protein levels are often elevated, reflecting disruption of the blood-brain barrier, while glucose levels may be decreased due to increased utilization by inflammatory cells.
Furthermore, blood cultures are essential for identifying the causative organism responsible for bacterial meningitis. Positive blood cultures provide definitive evidence of bacteremia, supporting the diagnosis of bacterial meningitis.
Neuroimaging studies, such as computed tomography (CT) or magnetic resonance imaging (MRI) of the brain, may be performed to assess for complications of bacterial meningitis, such as cerebral edema, hydrocephalus, or intracranial hemorrhage. These imaging modalities help guide management decisions and prognostication.
Based on the aforementioned clinical and laboratory findings, a diagnosis of bacterial meningitis can be established according to DSM-5 criteria. The presence of compatible clinical symptoms, along with supportive laboratory and imaging findings, confirms the diagnosis and guides appropriate management strategies.
In summary, the DSM-5 provides a structured framework for the diagnosis of bacterial meningitis, integrating clinical assessment, laboratory investigations, and neuroimaging studies to facilitate accurate identification and management of this potentially life-threatening condition. (Nursing Paper Example on Bacterial Meningitis: Understanding the Threat)
Treatment Regimens and Patient Education: Combatting Bacterial Meningitis
Effective management of bacterial meningitis requires a multi-faceted approach encompassing prompt initiation of antibiotic therapy, supportive care, and patient education to optimize outcomes and minimize complications.
Treatment Regimens:
- Antibiotic Therapy: Prompt initiation of empiric antibiotic therapy is essential in suspected cases of bacterial meningitis to prevent complications and improve outcomes. Empiric antibiotic selection is guided by local epidemiology and the patient’s age, immune status, and risk factors. Commonly used antibiotics include third-generation cephalosporins (e.g., ceftriaxone or cefotaxime) in combination with vancomycin to provide broad-spectrum coverage against common bacterial pathogens.
- Supportive Care: Supportive measures aim to alleviate symptoms, maintain vital functions, and prevent complications. Intravenous fluids are administered to ensure hydration and maintain electrolyte balance. Antipyretics such as acetaminophen or ibuprofen are prescribed to reduce fever and alleviate discomfort. Corticosteroids, such as dexamethasone, may be used adjunctively to mitigate inflammation and reduce the risk of neurologic sequelae, particularly in cases of suspected or confirmed bacterial meningitis caused by Streptococcus pneumoniae.
- Monitoring and Surveillance: Close monitoring of clinical status, vital signs, and neurological status is imperative in managing bacterial meningitis. Serial neurologic examinations and frequent assessments of consciousness, pupil reactivity, and motor function are conducted to detect changes indicative of worsening intracranial pressure or neurological compromise. Serial lumbar punctures may be performed to monitor CSF parameters and assess treatment response.
Patient Education:
- Vaccination: Educating patients and caregivers about the importance of vaccination against bacterial meningitis is paramount in preventing future occurrences. Encouraging adherence to recommended vaccination schedules, particularly for meningococcal conjugate vaccines and pneumococcal vaccines, can significantly reduce the risk of bacterial meningitis.
- Hygiene Practices: Promoting good hygiene practices, such as frequent handwashing with soap and water, covering coughs and sneezes, and avoiding close contact with individuals who are sick, can help prevent the spread of respiratory pathogens implicated in bacterial meningitis.
- Seeking Medical Attention: Emphasizing the importance of seeking prompt medical attention in cases of suspected bacterial meningitis is crucial. Educating patients and caregivers about the warning signs and symptoms of bacterial meningitis, such as fever, severe headache, neck stiffness, altered mental status, and rash, empowers them to recognize early signs of infection and seek timely medical evaluation and treatment.
Comprehensive management of bacterial meningitis entails a combination of antibiotic therapy, supportive care, and patient education. By implementing timely treatment regimens and empowering individuals with knowledge about preventive measures, we can effectively combat bacterial meningitis and improve outcomes for affected individuals. (Nursing Paper Example on Bacterial Meningitis: Understanding the Threat)