Nursing Paper Example on Carbon Monoxide Poisoning
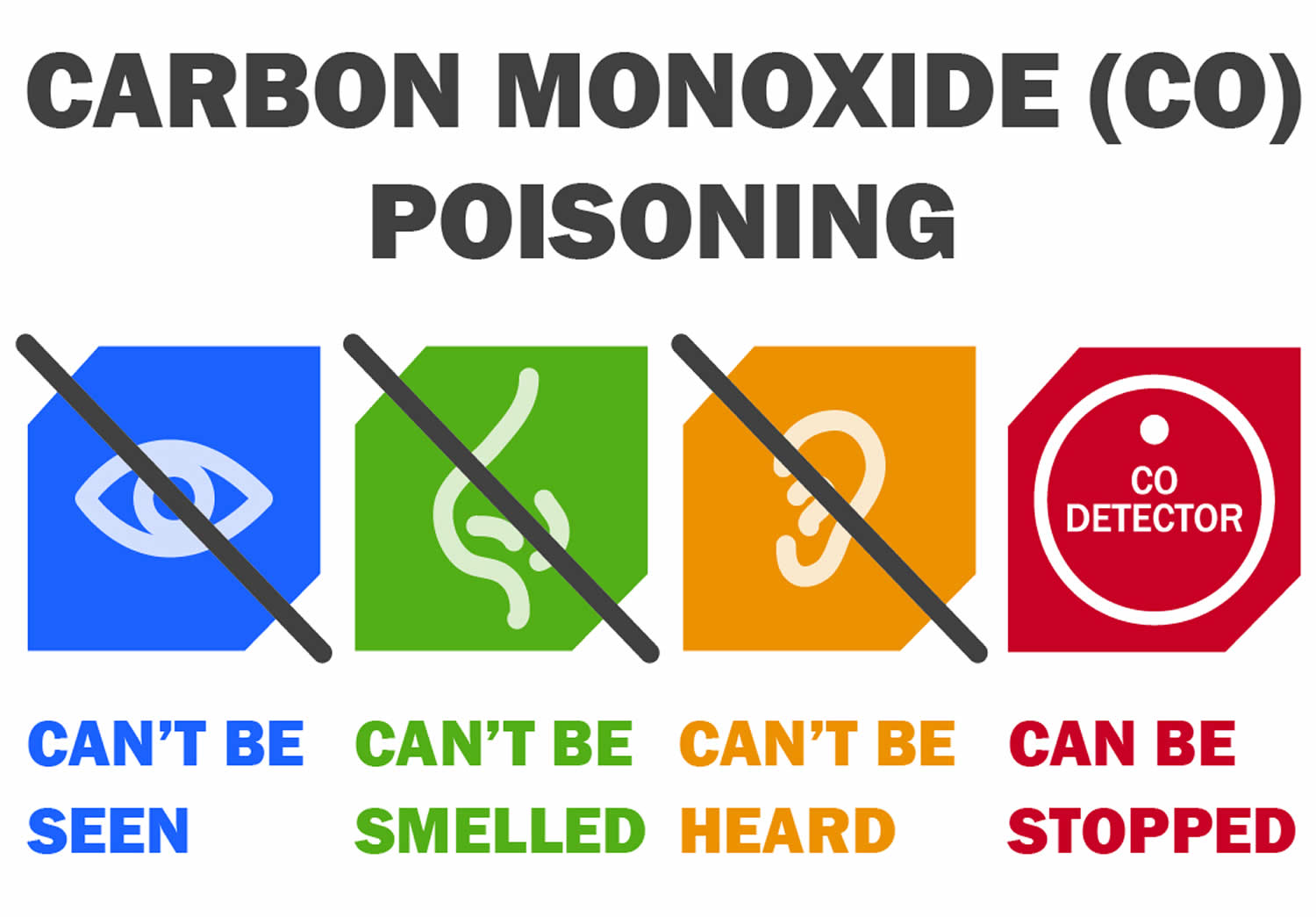
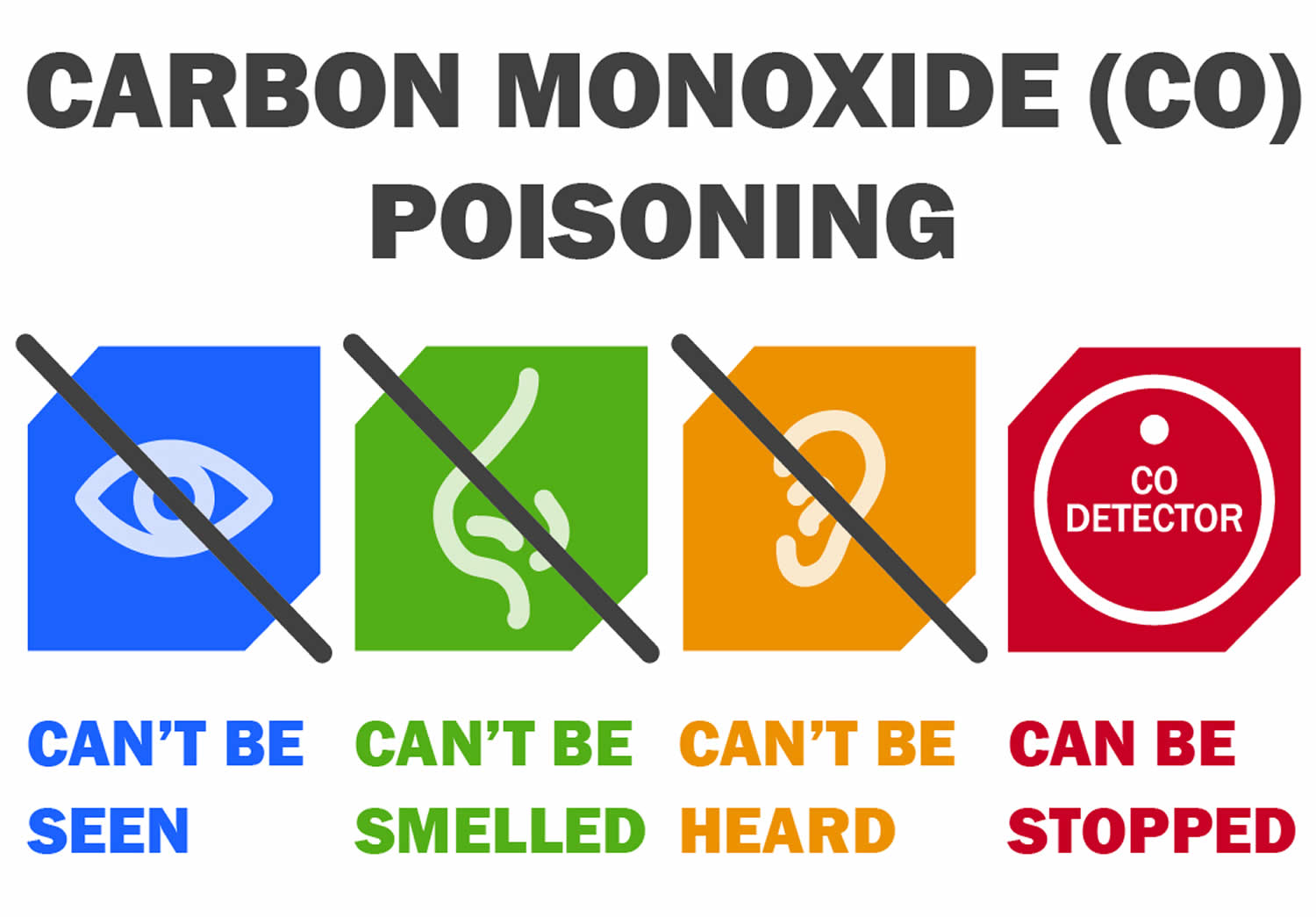
Carbon monoxide (CO) poisoning is a significant public health concern, often referred to as the “silent killer” due to its colorless, odorless, and tasteless nature. Exposure to CO can lead to severe health consequences, ranging from mild symptoms to life-threatening complications. Understanding the causes, signs, symptoms, etiology, pathophysiology, diagnostic criteria, treatment regimens, and patient education regarding CO poisoning is crucial for effective management and prevention. CO poisoning commonly occurs due to inhalation of CO gas produced by incomplete combustion of carbon-containing materials such as wood, gasoline, propane, and natural gas. Sources include malfunctioning household appliances (e.g., furnaces, water heaters), vehicle exhaust, and fires. The symptoms of CO poisoning can vary depending on the concentration and duration of exposure, making it imperative to recognize and address this silent threat promptly. (Nursing Paper Example on Carbon Monoxide Poisoning)
Causes
Carbon monoxide (CO) poisoning occurs when individuals inhale CO gas, a byproduct of incomplete combustion of carbon-containing materials. Common sources of CO include malfunctioning household appliances such as furnaces, water heaters, and gas stoves. Improperly ventilated or enclosed spaces can lead to CO buildup, increasing the risk of poisoning. Additionally, vehicle exhaust, generators, and fires produce CO, posing a threat in both indoor and outdoor environments.
Inadequate maintenance of combustion appliances, including blocked vents or flues, can contribute to CO accumulation. Poorly maintained chimneys and blocked or damaged exhaust systems can also lead to CO leaks. Furthermore, using fuel-burning appliances in poorly ventilated areas, such as using a gas stove for heating or running a generator inside a closed garage, can result in dangerous levels of CO.
Certain occupational settings pose an increased risk of CO exposure. Workers in industries such as mining, firefighting, and construction may encounter elevated CO levels due to machinery operation, vehicle exhaust, or confined spaces with inadequate ventilation.
Environmental factors can exacerbate CO poisoning risks. During natural disasters such as hurricanes or winter storms, power outages may prompt individuals to use alternative heating sources, increasing the likelihood of CO exposure if not used safely. Additionally, living in urban areas with heavy traffic or proximity to industrial facilities can elevate ambient CO levels, contributing to overall exposure risk.
Lastly, intentional CO exposure, whether through suicide attempts or misuse of equipment such as charcoal grills or portable generators indoors, is a concerning cause of CO poisoning. Understanding the diverse sources and circumstances that can lead to CO exposure is essential for implementing effective prevention strategies and mitigating the risks associated with this silent yet deadly gas. (Nursing Paper Example on Carbon Monoxide Poisoning)
Signs and Symptoms
Carbon monoxide (CO) poisoning presents with a wide range of signs and symptoms that can vary in severity depending on the concentration and duration of exposure. Early symptoms of CO poisoning are often nonspecific and may resemble flu-like illness, making diagnosis challenging without a high index of suspicion.
Headache is one of the most common early symptoms of CO poisoning and is often described as dull, persistent, and worsening over time. Dizziness and lightheadedness are also prevalent, accompanied by a feeling of weakness or fatigue. Nausea and vomiting may occur, further contributing to the flu-like presentation.
As CO levels rise or exposure continues, individuals may experience more severe symptoms. Cognitive impairment is common, manifesting as confusion, difficulty concentrating, or memory problems. Visual disturbances, such as blurred vision, may also occur due to reduced oxygen delivery to the optic nerve.
Cardiovascular symptoms can manifest as chest pain or palpitations, reflecting the heart’s increased workload in response to tissue hypoxia. Shortness of breath and difficulty breathing may occur, particularly in individuals with underlying respiratory conditions.
Neurological symptoms are concerning and may indicate more severe CO poisoning. These include altered mental status, ranging from mild confusion to coma, and neurological deficits such as weakness, tremors, or seizures.
In severe cases of CO poisoning, individuals may experience loss of consciousness or respiratory arrest, requiring immediate medical intervention. The presence of cherry-red skin coloration, although rare, is a classic but not universally observed sign of severe CO poisoning.
It is essential to recognize these signs and symptoms promptly, especially in cases of suspected CO exposure, to initiate appropriate management and prevent further complications. Rapid recognition and treatment can significantly impact patient outcomes and reduce the risk of long-term sequelae associated with CO poisoning. (Nursing Paper Example on Carbon Monoxide Poisoning)
:max_bytes(150000):strip_icc()/VWH-JessicaOlah-CommonSymptomsofCarbonMonoxidePoisoning-Standard-460087eaa2ad4058af35e4606caabe07.jpg)
Etiology
Carbon monoxide (CO) poisoning occurs when individuals are exposed to elevated levels of CO gas, leading to the formation of carboxyhemoglobin (COHb) in the bloodstream. CO is produced through incomplete combustion of carbon-containing materials, such as wood, gasoline, propane, and natural gas. The primary sources of CO exposure include malfunctioning household appliances, vehicle exhaust, fires, and occupational settings where combustion processes occur.
Upon inhalation, CO rapidly diffuses across the alveolar-capillary membrane in the lungs and enters the bloodstream. CO has a high affinity for hemoglobin, the oxygen-carrying protein in red blood cells, and forms a stable bond with hemoglobin molecules to create COHb. This process interferes with the normal oxygen transport function of hemoglobin, reducing the blood’s oxygen-carrying capacity and impairing oxygen delivery to tissues and organs.
The formation of COHb disrupts the oxygen dissociation curve, shifting it to the left and reducing the release of oxygen to tissues, even in the presence of adequate arterial oxygen tension. This leads to tissue hypoxia, particularly in organs with high oxygen demand, such as the brain, heart, and lungs.
In addition to its affinity for hemoglobin, CO can also directly affect cellular function and metabolism. CO inhibits cytochrome c oxidase, a key enzyme involved in the electron transport chain of mitochondrial respiration. By interfering with cellular respiration, CO disrupts ATP production and cellular metabolism, contributing to tissue hypoxia and cellular dysfunction.
Furthermore, CO induces oxidative stress and inflammation by generating reactive oxygen species (ROS) and activating inflammatory pathways. ROS can cause cellular damage and lipid peroxidation, further exacerbating tissue injury and organ dysfunction.
Overall, the etiology of CO poisoning involves complex interactions between CO gas, hemoglobin, cellular metabolism, oxidative stress, and inflammatory processes, ultimately leading to systemic effects and clinical manifestations of CO toxicity. (Nursing Paper Example on Carbon Monoxide Poisoning)
Pathophysiology
Carbon monoxide (CO) poisoning disrupts normal cellular oxygen metabolism, leading to systemic hypoxia and tissue injury. Upon inhalation, CO rapidly binds to hemoglobin, forming carboxyhemoglobin (COHb), which has a higher affinity for oxygen than hemoglobin. This results in the displacement of oxygen molecules from hemoglobin, reducing the blood’s oxygen-carrying capacity and impairing oxygen delivery to tissues and organs.
The formation of COHb shifts the oxygen dissociation curve to the left, inhibiting the release of oxygen to tissues, even in the presence of adequate arterial oxygen tension. This leads to tissue hypoxia, particularly in organs with high oxygen demand, such as the brain, heart, and lungs. Hypoxic injury can result in cellular dysfunction, oxidative stress, and inflammatory responses.
In addition to its effects on hemoglobin, CO can directly impact cellular metabolism and function. CO inhibits cytochrome c oxidase, a critical enzyme in the electron transport chain of mitochondrial respiration. By disrupting cellular respiration, CO impairs adenosine triphosphate (ATP) production and cellular metabolism, further contributing to tissue hypoxia and cellular dysfunction.
Furthermore, CO induces oxidative stress by generating reactive oxygen species (ROS), leading to cellular damage, lipid peroxidation, and mitochondrial dysfunction. ROS-mediated damage exacerbates tissue injury and triggers inflammatory responses, amplifying the pathophysiological effects of CO poisoning.
The central nervous system (CNS) is particularly vulnerable to CO toxicity due to its high oxygen demand and susceptibility to hypoxic injury. CO poisoning can cause cerebral edema, neuronal damage, and demyelination, leading to neurological deficits and long-term cognitive impairment.
Overall, the pathophysiology of CO poisoning involves complex interactions between CO, hemoglobin, cellular metabolism, oxidative stress, and inflammatory processes, ultimately resulting in systemic hypoxia, tissue injury, and neurological sequelae. Understanding the underlying mechanisms of CO toxicity is essential for developing effective treatment strategies and minimizing the long-term consequences of CO exposure. (Nursing Paper Example on Carbon Monoxide Poisoning)
DMS-5 Diagnosis
Diagnosing carbon monoxide (CO) poisoning involves a comprehensive assessment of clinical history, symptoms, laboratory findings, and imaging studies. The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), does not provide specific diagnostic criteria for CO poisoning; however, healthcare providers utilize a combination of clinical judgment and objective measures to establish a diagnosis.
A thorough history is crucial in identifying potential sources of CO exposure, such as recent use of fuel-burning appliances, occupational hazards, or environmental factors. Patients may report symptoms consistent with CO poisoning, including headache, dizziness, nausea, and confusion, which should prompt further evaluation.
Physical examination findings may vary depending on the severity of CO poisoning. Patients may exhibit signs of hypoxia, such as tachypnea, tachycardia, and cyanosis. Neurological examination may reveal altered mental status, focal deficits, or signs of encephalopathy.
Arterial or venous blood gas analysis is a valuable tool in confirming the diagnosis of CO poisoning. Elevated levels of carboxyhemoglobin (COHb) in the blood indicate recent exposure to CO. However, it is important to note that COHb levels may decrease rapidly over time, especially with the administration of supplemental oxygen, underscoring the importance of early testing.
Imaging studies such as brain magnetic resonance imaging (MRI) may be performed in severe cases to assess for cerebral edema, ischemic changes, or other neurologic abnormalities associated with CO poisoning.
The differential diagnosis for CO poisoning includes other conditions that present with similar symptoms, such as influenza, viral syndromes, migraine headaches, and other toxic exposures. Healthcare providers must consider these differential diagnoses and use clinical judgment in ruling out alternative etiologies.
Overall, the diagnosis of CO poisoning requires a high index of suspicion, thorough clinical evaluation, and appropriate laboratory and imaging studies to confirm the presence of CO exposure and guide treatment interventions. Early recognition and management are essential to prevent complications and mitigate the long-term effects of CO toxicity. (Nursing Paper Example on Carbon Monoxide Poisoning)
Treatment Regimens and Patient Education
Management of carbon monoxide (CO) poisoning focuses on prompt removal from the source of exposure, administration of supplemental oxygen, and consideration of hyperbaric oxygen therapy (HBOT) in severe cases. Additionally, patient education plays a crucial role in preventing future incidents and promoting safety measures to minimize the risk of CO exposure.
Immediate Actions:
- Removal from the Source: The first step in treating CO poisoning is to remove the patient from the contaminated environment to prevent further exposure.
- Supplemental Oxygen: Administering high-flow oxygen via a non-rebreather mask or endotracheal tube increases the elimination half-life of CO and facilitates the displacement of CO from hemoglobin, restoring tissue oxygenation.
- Monitoring: Continuous monitoring of vital signs, including pulse oximetry, is essential to assess the patient’s response to treatment and detect any deterioration in clinical status.
Hyperbaric Oxygen Therapy (HBOT):
- In severe cases of CO poisoning, particularly when patients present with altered mental status, neurologic deficits, or signs of tissue hypoxia, hyperbaric oxygen therapy (HBOT) is recommended.
- HBOT involves placing the patient in a hyperbaric chamber and administering 100% oxygen at increased atmospheric pressure. This accelerates the elimination of CO from the bloodstream and tissues, promotes tissue oxygenation, and reduces the risk of long-term neurological sequelae.
Patient Education:
- Prevention Strategies: Educating patients and their families about the importance of proper ventilation, regular maintenance of household appliances (e.g., furnaces, water heaters), and installation of CO detectors can help prevent CO exposure.
- CO Detector Use: Encouraging the installation of CO detectors in homes and other enclosed spaces where combustion appliances are used can provide early warning of CO leaks and prompt evacuation.
- Safe Practices: Advising against the use of fuel-burning appliances, such as charcoal grills or portable generators, indoors or in enclosed spaces can prevent CO buildup and minimize the risk of poisoning.
- Emergency Preparedness: Educating patients about the signs and symptoms of CO poisoning, emphasizing the importance of seeking immediate medical attention if exposure is suspected, and knowing how to respond in case of an emergency can save lives.
Overall, a multidisciplinary approach involving healthcare providers, emergency responders, and public health agencies is essential in the management and prevention of CO poisoning. By implementing effective treatment regimens and providing comprehensive patient education, healthcare professionals can mitigate the impact of CO toxicity and empower individuals to safeguard against future exposures. (Nursing Paper Example on Carbon Monoxide Poisoning)
Conclusion
Carbon monoxide (CO) poisoning is a serious health concern that necessitates prompt recognition, appropriate treatment, and comprehensive patient education to mitigate its potentially life-threatening consequences. By understanding the diverse sources and causes of CO exposure, recognizing the varied signs and symptoms, and employing effective treatment regimens such as supplemental oxygen and hyperbaric oxygen therapy (HBOT) in severe cases, healthcare providers can significantly impact patient outcomes and prevent long-term complications. Additionally, emphasizing the importance of preventive measures such as proper ventilation, regular maintenance of household appliances, installation of CO detectors, and safe practices can empower individuals to reduce their risk of CO exposure and protect themselves and their families. Through a collaborative effort involving healthcare professionals, emergency responders, and public health initiatives, we can raise awareness, improve recognition, and ultimately minimize the burden of CO poisoning on public health. (Nursing Paper Example on Carbon Monoxide Poisoning)
References
https://www.ncbi.nlm.nih.gov/books/NBK430740/
Do you need a similar assignment done for you from scratch? Order now!
Use Discount Code "Newclient" for a 15% Discount!


:max_bytes(150000):strip_icc()/VWH-JessicaOlah-CommonSymptomsofCarbonMonoxidePoisoning-Standard-460087eaa2ad4058af35e4606caabe07.jpg)


