Nursing Paper Example on Congestive Heart Disease
Nursing Paper Example on Congestive Heart Disease
 Causes
Causes
Congestive heart disease arises from a myriad of factors, each contributing to the impaired functioning of the heart. One primary cause is coronary artery disease (CAD), characterized by the narrowing or blockage of coronary arteries that supply blood to the heart muscle. CAD often results from the buildup of plaque, composed of cholesterol and other substances, within the arterial walls. As plaque accumulates, it restricts blood flow to the heart, leading to myocardial ischemia and eventual damage.
Hypertension, or high blood pressure, is another significant contributor to congestive heart disease. Prolonged hypertension exerts excessive strain on the heart, causing it to pump harder to circulate blood throughout the body. Over time, this increased workload can weaken the heart muscle, impairing its ability to contract and pump blood effectively.
Heart valve disorders represent another common cause of congestive heart disease. Conditions such as aortic stenosis, mitral regurgitation, and mitral stenosis can disrupt the flow of blood within the heart chambers, leading to inefficient circulation and eventual heart failure.
Congenital heart defects, present at birth, can also predispose individuals to congestive heart disease. These structural abnormalities in the heart’s chambers or valves can impede blood flow and strain the heart’s pumping function.
Furthermore, cardiomyopathy, a disease of the heart muscle, can contribute to congestive heart disease. Various forms of cardiomyopathy, including dilated cardiomyopathy, hypertrophic cardiomyopathy, and restrictive cardiomyopathy, can weaken the heart muscle and impair its ability to contract effectively.
Lifestyle factors such as smoking, obesity, and a sedentary lifestyle also play a significant role in the development of congestive heart disease. Smoking damages blood vessels, while obesity and physical inactivity contribute to hypertension, diabetes, and dyslipidemia, all of which are risk factors for heart failure.
In summary, congestive heart disease arises from a complex interplay of genetic predisposition, environmental factors, and lifestyle choices, highlighting the importance of comprehensive prevention and management strategies. (Nursing Paper Example on Congestive Heart Disease)
Signs and Symptoms
Etiology
The etiology of congestive heart disease encompasses a complex interplay of genetic predisposition, environmental factors, and lifestyle choices, each contributing to the development and progression of the condition.
Genetic factors play a significant role in predisposing individuals to congestive heart disease. Family history of cardiovascular disorders, including coronary artery disease, hypertension, and cardiomyopathy, can increase one’s susceptibility to developing heart failure. Genetic mutations affecting cardiac structure and function may also contribute to the pathogenesis of congestive heart disease.
Environmental influences, such as exposure to toxins and pollutants, can exacerbate cardiac dysfunction and hasten the progression of heart failure. Chronic exposure to cigarette smoke, air pollution, and industrial chemicals can promote inflammation, oxidative stress, and endothelial dysfunction, impairing cardiovascular health and predisposing individuals to heart failure.
Furthermore, lifestyle choices significantly impact the development of congestive heart disease. Sedentary behavior, poor dietary habits, excessive alcohol consumption, and tobacco use are all modifiable risk factors that contribute to the development of cardiovascular disease. A diet high in saturated fats, cholesterol, and sodium can promote atherosclerosis and hypertension, while physical inactivity exacerbates obesity, insulin resistance, and dyslipidemia, all of which are risk factors for heart failure.
Chronic conditions such as diabetes mellitus and chronic kidney disease also contribute to the etiology of congestive heart disease. These comorbidities exert systemic effects on cardiovascular health, promoting endothelial dysfunction, inflammation, and fibrosis, all of which can impair cardiac function and predispose individuals to heart failure.
In summary, the etiology of congestive heart disease is multifactorial, involving a complex interplay of genetic predisposition, environmental influences, and lifestyle factors. Understanding these underlying mechanisms is crucial for implementing targeted prevention and management strategies to mitigate the burden of heart failure on individuals and society. (Nursing Paper Example on Congestive Heart Disease)
Pathophysiology
The pathophysiology of congestive heart disease involves a cascade of events that disrupts the heart’s ability to effectively pump blood throughout the body, leading to systemic manifestations of heart failure.
One primary mechanism underlying congestive heart disease is impaired myocardial contractility. Damage to the heart muscle, often resulting from ischemic injury or chronic pressure overload, compromises the heart’s ability to contract forcefully, impairing its pumping function.
Another hallmark feature of congestive heart disease is neurohormonal activation. In response to reduced cardiac output and perfusion pressure, the sympathetic nervous system is activated, leading to increased catecholamine release. This results in vasoconstriction, sodium and water retention, and increased cardiac workload, further exacerbating cardiac dysfunction.
Additionally, the renin-angiotensin-aldosterone system (RAAS) is upregulated in congestive heart disease. Decreased renal perfusion stimulates renin release, initiating a cascade of events that culminates in angiotensin II-mediated vasoconstriction and aldosterone secretion, promoting sodium and water retention and exacerbating fluid overload.
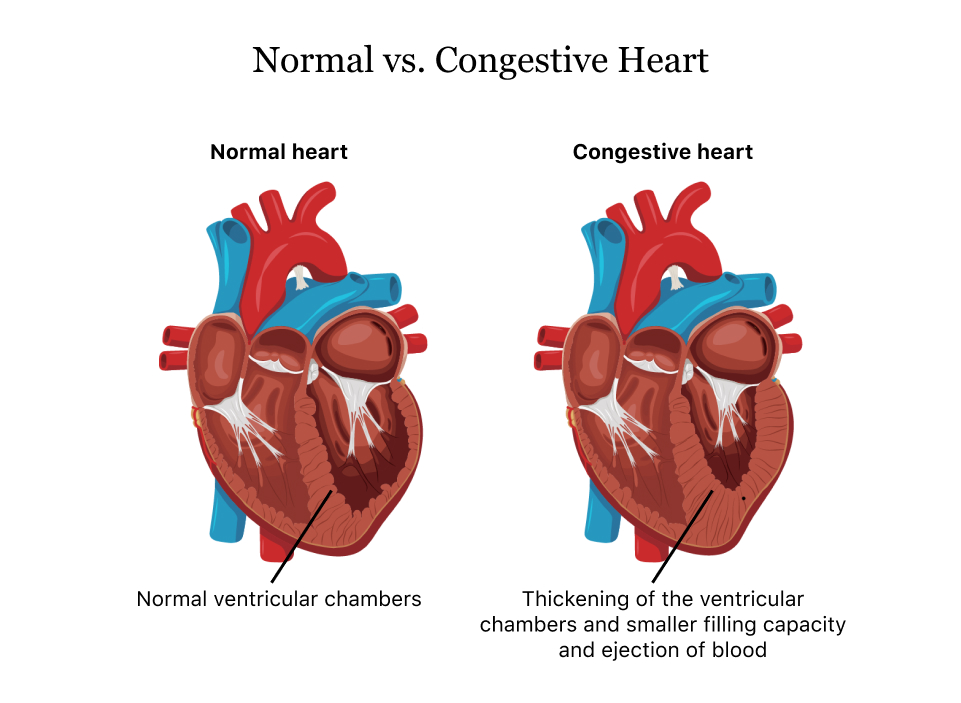
Furthermore, ventricular remodeling plays a pivotal role in the progression of congestive heart disease. Chronic pressure and volume overload trigger maladaptive changes in cardiac structure and function, including hypertrophy, fibrosis, and chamber dilation. These structural alterations further compromise cardiac function, perpetuating the cycle of heart failure progression.
Inflammatory and oxidative stress pathways also contribute to the pathophysiology of congestive heart disease. Endothelial dysfunction, inflammation, and oxidative damage promote atherosclerosis, endothelial injury, and myocardial fibrosis, exacerbating cardiac dysfunction and impairing myocardial contractility.
In summary, the pathophysiology of congestive heart disease involves a complex interplay of hemodynamic, neurohormonal, inflammatory, and structural alterations, each contributing to the progressive decline in cardiac function observed in heart failure. Understanding these underlying mechanisms is essential for developing targeted therapeutic interventions to mitigate the burden of congestive heart disease on affected individuals. (Nursing Paper Example on Congestive Heart Disease)
DSM-5 Diagnosis
Treatment Regimens and Patient Education
Effective management of congestive heart disease requires a comprehensive approach encompassing pharmacological interventions, lifestyle modifications, and patient education. Pharmacotherapy plays a central role in symptom control and disease progression. Diuretics, such as furosemide, help alleviate fluid retention by increasing urine output, relieving symptoms of congestion. ACE inhibitors and angiotensin receptor blockers (ARBs) improve cardiac function and reduce mortality by inhibiting the renin-angiotensin-aldosterone system, thereby decreasing vasoconstriction and fluid retention. Beta-blockers, like carvedilol, help regulate heart rate and blood pressure, reducing myocardial workload. Aldosterone antagonists, such as spironolactone, further enhance diuresis and mitigate cardiac remodeling. In advanced cases, vasodilators like hydralazine and nitrates may be employed to improve cardiac output.
Concomitant with pharmacotherapy, lifestyle modifications are crucial for managing congestive heart disease. Patients are advised to adopt a heart-healthy diet low in sodium, saturated fats, and cholesterol to reduce fluid retention and lower blood pressure. Regular physical activity, tailored to individual capabilities, strengthens the heart muscle and improves overall cardiovascular health. Smoking cessation and limiting alcohol intake are imperative to mitigate further cardiac damage and enhance treatment efficacy. Weight management through portion control and calorie restriction is essential to alleviate strain on the heart and improve functional capacity.
Patient education plays a pivotal role in empowering individuals with congestive heart disease to actively participate in their care. Healthcare providers should educate patients about their condition, emphasizing the importance of medication adherence, including proper dosing and timing, to optimize treatment efficacy. Patients should be educated about monitoring and recognizing symptoms of worsening heart failure, such as increasing shortness of breath or swelling, and instructed on when to seek medical attention. Additionally, patients should be counseled on dietary modifications, such as adhering to a low-sodium diet, and encouraged to engage in regular physical activity within their abilities. Providing emotional support and addressing concerns about prognosis and lifestyle adjustments are also integral components of patient education, fostering a collaborative approach to managing congestive heart disease and improving patient outcomes. (Nursing Paper Example on Congestive Heart Disease)



