Nursing Paper Example on Guillain-Barré Syndrome: Understanding a Neurological Disorder
/in Assignment Help, Assignment Help Nursing, BLOG, Homework Help, Nursing Exam Help, Nursing Paper Help, Solved Nursing Essays /by Aimee GraceNursing Paper Example on Guillain-Barré Syndrome: Understanding a Neurological Disorder
Guillain-Barré Syndrome (GBS) is a neurological disorder that affects the peripheral nervous system, causing muscle weakness and paralysis in severe cases. While rare, GBS can have profound implications for affected individuals, necessitating a comprehensive understanding of its causes, symptoms, and management strategies. By exploring various facets of GBS, including its etiology, pathophysiology, diagnosis, treatment regimens, and patient education, we can enhance awareness and knowledge about GBS, enabling healthcare professionals and patients alike to better recognize, manage, and cope with this condition. Through this exploration, we seek to shed light on the complexities of GBS and highlight the importance of early detection, prompt intervention, and ongoing support for individuals living with this neurological disorder. (Nursing Paper Example on Guillain-Barré Syndrome: Understanding a Neurological Disorder)
Causes
Guillain-Barré Syndrome (GBS) typically arises following an immune response triggered by various factors, notably preceding infections and vaccinations. One of the most commonly associated infections is Campylobacter jejuni, a bacterium often found in undercooked poultry and contaminated water sources. Studies have shown that up to 30% of GBS cases are preceded by a Campylobacter jejuni infection.
Furthermore, viral infections such as cytomegalovirus, Epstein-Barr virus, and Zika virus have also been linked to GBS. These viruses can provoke an abnormal immune response, leading to the development of GBS in susceptible individuals.
In addition to infections, vaccinations have been implicated as potential triggers for GBS. Notably, influenza and swine flu vaccines have been associated with an increased risk of GBS, although the absolute risk remains low. It is believed that the immune response elicited by these vaccines may sometimes cross-react with peripheral nerves, leading to the development of GBS.
Other potential risk factors for GBS include autoimmune diseases, such as systemic lupus erythematosus and rheumatoid arthritis, as well as certain medications, including some antibiotics and antiviral drugs. However, the precise mechanisms by which these factors contribute to the development of GBS are not fully understood.
Overall, GBS is thought to result from a complex interplay between genetic predisposition, environmental triggers, and immune dysregulation. While the exact cause of GBS remains elusive in many cases, identifying and addressing potential triggers, such as preceding infections and vaccinations, can aid in the prevention and management of this neurological disorder. Further research is needed to elucidate the underlying mechanisms of GBS and develop targeted interventions to mitigate its impact on affected individuals. (Nursing Paper Example on Guillain-Barré Syndrome: Understanding a Neurological Disorder)
Signs and Symptoms
Guillain-Barré Syndrome (GBS) manifests with a range of signs and symptoms, typically beginning with sensory abnormalities and muscle weakness that gradually progress over days to weeks. The hallmark feature of GBS is ascending weakness, starting in the legs and spreading symmetrically to the arms and upper body. This weakness may initially present as difficulty walking or climbing stairs and can progress to the point of complete paralysis in severe cases.
Sensory disturbances are also common in GBS, including tingling sensations (paresthesias), numbness, and heightened sensitivity to touch or pain. These sensory abnormalities often accompany muscle weakness and may precede motor symptoms.
In addition to weakness and sensory changes, individuals with GBS may experience autonomic dysfunction, affecting various bodily functions regulated by the autonomic nervous system. Symptoms of autonomic dysfunction may include fluctuations in blood pressure and heart rate, abnormal sweating, and gastrointestinal disturbances such as constipation or urinary retention.
Furthermore, respiratory muscle weakness is a serious complication of GBS that can lead to respiratory failure and necessitate mechanical ventilation in severe cases. Individuals with GBS may exhibit signs of respiratory distress, such as shortness of breath, shallow breathing, or cyanosis (bluish discoloration of the skin and mucous membranes).
As GBS progresses, affected individuals may become increasingly debilitated, requiring assistance with daily activities and mobility. The severity and progression of symptoms can vary widely among individuals with GBS, ranging from mild weakness to complete paralysis. Prompt recognition and management of GBS are crucial to prevent complications and optimize outcomes for affected individuals. Early signs of GBS should prompt immediate medical evaluation to initiate appropriate treatment and supportive care. (Nursing Paper Example on Guillain-Barré Syndrome: Understanding a Neurological Disorder)

Etiology
The etiology of Guillain-Barré Syndrome (GBS) remains incompletely understood, but it is believed to involve a complex interplay of genetic predisposition, environmental triggers, and immune dysregulation. While the precise mechanisms underlying the development of GBS are not fully elucidated, several theories have been proposed to explain its pathogenesis.
One prominent theory suggests that GBS is an autoimmune disorder, wherein the body’s immune system mistakenly attacks the peripheral nerves, leading to nerve damage and subsequent neurological symptoms. This autoimmune response is thought to be triggered by preceding infections or vaccinations, which stimulate the immune system to produce antibodies that cross-react with components of the peripheral nerves. These antibodies target specific proteins or gangliosides located on the surface of nerve cells, resulting in inflammation and demyelination of peripheral nerves.
Another proposed mechanism involves molecular mimicry, wherein infectious agents share structural similarities with peripheral nerve components, leading to immune cross-reactivity and nerve damage. For example, Campylobacter jejuni, a common bacterial pathogen associated with GBS, possesses lipopolysaccharides that mimic gangliosides found on nerve cells, potentially triggering an immune response against both the bacteria and the peripheral nerves.
Genetic factors may also play a role in predisposing individuals to GBS. Certain genetic variations have been associated with increased susceptibility to autoimmune diseases and aberrant immune responses, which could contribute to the development of GBS in genetically susceptible individuals.
Moreover, environmental factors, such as infections and vaccinations, are known to precipitate GBS in susceptible individuals. Infections with bacteria, viruses, or other pathogens can trigger an immune response that culminates in the development of GBS. Similarly, vaccinations, particularly those against influenza and swine flu, have been implicated as potential triggers for GBS, although the absolute risk remains low.
Overall, GBS is likely a multifactorial disorder with a complex etiology involving interactions between genetic predisposition, environmental triggers, and immune dysregulation. Further research is needed to elucidate the underlying mechanisms and identify potential targets for therapeutic interventions aimed at preventing or mitigating the development of GBS. (Nursing Paper Example on Guillain-Barré Syndrome: Understanding a Neurological Disorder)
Pathophysiology
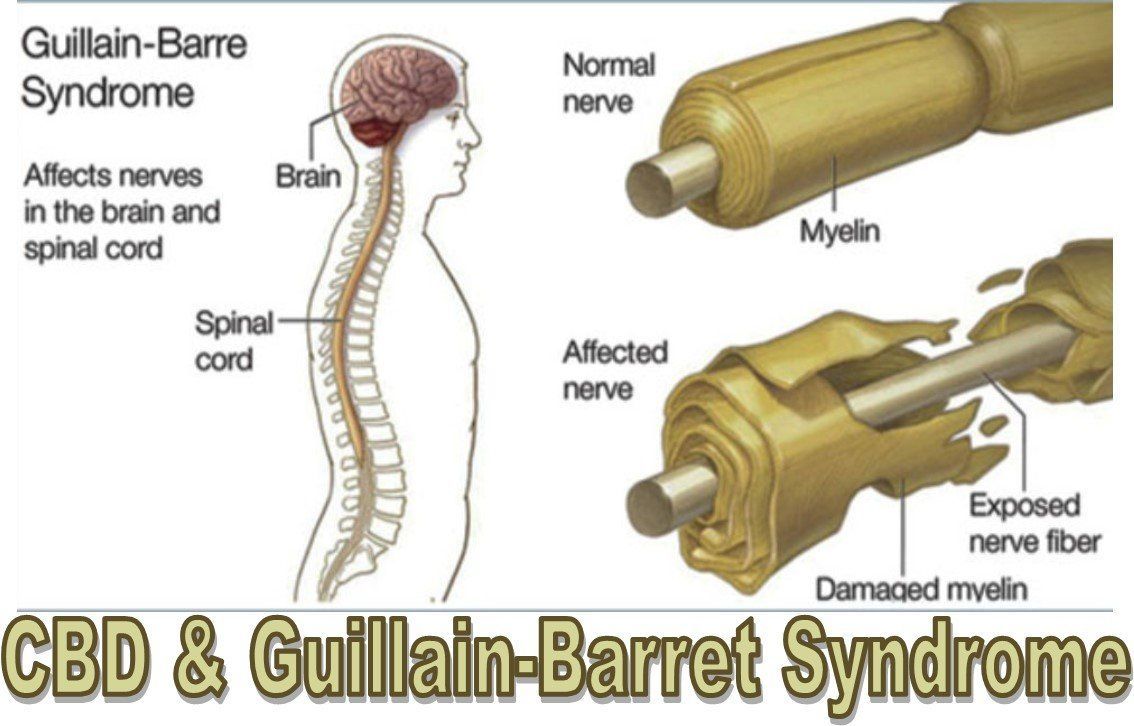
The pathophysiology of Guillain-Barré Syndrome (GBS) involves an aberrant immune response targeting the peripheral nervous system, leading to inflammation, demyelination, and subsequent nerve dysfunction. This autoimmune-mediated damage primarily affects the myelin sheath, the fatty substance that surrounds and insulates nerve fibers, disrupting nerve signal transmission and impairing motor and sensory function.
The initial trigger for the immune response in GBS is often an infection or vaccination, which stimulates the production of antibodies and activates immune cells such as T lymphocytes. These immune cells infiltrate the peripheral nerves, where they release pro-inflammatory cytokines and other mediators that promote inflammation and recruit additional immune cells to the site of injury.
Inflammation within the peripheral nerves leads to damage to the myelin sheath, a process known as demyelination. Demyelination impairs the ability of nerve fibers to conduct electrical impulses efficiently, resulting in slowed or blocked nerve conduction. This disruption of nerve signal transmission manifests clinically as muscle weakness, sensory abnormalities, and other neurological symptoms characteristic of GBS.
In addition to demyelination, GBS can also involve damage to the axons, the long projections of nerve cells responsible for transmitting nerve impulses. Axonal injury may occur secondary to inflammation or direct immune-mediated attack, leading to further impairment of nerve function and contributing to the severity of symptoms in some cases.
The pathophysiological mechanisms underlying GBS are heterogeneous, with variations in the extent and distribution of nerve damage observed among affected individuals. Subtypes of GBS, such as acute inflammatory demyelinating polyneuropathy (AIDP) and acute motor axonal neuropathy (AMAN), exhibit distinct pathophysiological features, further highlighting the complexity of the disorder.
Overall, the pathophysiology of GBS involves a cascade of immune-mediated events leading to inflammation, demyelination, and axonal injury within the peripheral nervous system. Understanding these underlying mechanisms is essential for developing targeted therapeutic interventions aimed at modulating the immune response, promoting nerve regeneration, and improving outcomes for individuals affected by GBS. (Nursing Paper Example on Guillain-Barré Syndrome: Understanding a Neurological Disorder)
DSM-5 Diagnosis
Guillain-Barré Syndrome (GBS) is primarily diagnosed based on clinical presentation, neurological examination findings, and supportive diagnostic tests. While the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), is not specifically designed to diagnose neurological disorders like GBS, certain criteria and guidelines can aid in the diagnostic process.

The DSM-5 criteria for GBS encompass the presence of rapidly progressive weakness in more than one limb, accompanied by absent or diminished deep tendon reflexes. Additionally, the absence of alternative explanations for weakness, such as spinal cord compression or botulism, is necessary to establish the diagnosis of GBS.
Neurological examination findings consistent with GBS may include symmetrical weakness, sensory abnormalities, and autonomic dysfunction. Reflexes may be diminished or absent, reflecting the underlying peripheral nerve involvement characteristic of GBS.
Supportive diagnostic tests play a crucial role in confirming the diagnosis of GBS and differentiating it from other neurological conditions with similar clinical presentations. Nerve conduction studies (NCS) and electromyography (EMG) can demonstrate characteristic findings such as nerve conduction slowing and abnormal spontaneous activity, indicative of demyelination and axonal injury within the peripheral nerves.
Cerebrospinal fluid (CSF) analysis may reveal an elevated protein level without pleocytosis, a hallmark feature of GBS known as albuminocytological dissociation. This finding reflects disruption of the blood-nerve barrier and leakage of protein into the CSF, supporting the diagnosis of GBS.
Imaging studies such as magnetic resonance imaging (MRI) of the spine or nerve roots may be performed to rule out alternative diagnoses or complications of GBS, such as nerve root compression or spinal cord lesions.
In summary, while the DSM-5 does not provide specific diagnostic criteria for GBS, clinical evaluation, neurological examination, and supportive diagnostic tests are essential components of the diagnostic process. By integrating these findings, healthcare providers can establish a diagnosis of GBS and initiate appropriate management and treatment strategies for affected individuals. (Nursing Paper Example on Guillain-Barré Syndrome: Understanding a Neurological Disorder)
Treatment Regimens and Patient Education
Effective management of Guillain-Barré Syndrome (GBS) involves a multidisciplinary approach aimed at reducing the severity of symptoms, preventing complications, and promoting recovery. Treatment regimens for GBS typically consist of supportive care, immunomodulatory therapies, and rehabilitation interventions, tailored to the individual needs and clinical course of each patient.
Supportive Care: Supportive care plays a vital role in managing the complications of GBS and ensuring optimal outcomes for affected individuals. This includes close monitoring of respiratory function, as respiratory muscle weakness can lead to respiratory failure and necessitate mechanical ventilation. Early recognition of respiratory distress and timely intervention with ventilatory support can prevent respiratory complications and improve patient outcomes.
Other aspects of supportive care may include monitoring and management of autonomic dysfunction, nutritional support, and pain management. Addressing the psychological and emotional needs of patients and providing psychosocial support can also contribute to overall well-being and recovery.
Immunomodulatory Therapies: Immunomodulatory therapies are aimed at modulating the immune response in GBS to reduce inflammation and prevent further nerve damage. Intravenous immunoglobulin (IVIG) and plasma exchange (also known as plasmapheresis) are the mainstay treatments for GBS, both of which have been shown to accelerate recovery and improve outcomes.
IVIG administration involves infusing a high dose of immunoglobulins derived from pooled human plasma, which helps modulate the immune response and suppress inflammation. Plasma exchange entails removing and replacing the patient’s plasma to eliminate harmful antibodies and inflammatory mediators, thereby attenuating the immune response.
The choice between IVIG and plasma exchange depends on various factors, including the availability of resources, patient preferences, and clinical considerations. Both treatments have demonstrated efficacy in reducing the duration of symptoms and improving functional outcomes in patients with GBS.
Rehabilitation Interventions: Rehabilitation interventions are essential components of GBS management, aimed at optimizing functional recovery and enhancing quality of life. Physical therapy focuses on improving muscle strength, flexibility, and mobility through exercises and rehabilitation techniques tailored to the individual’s abilities and goals.
Occupational therapy helps individuals regain independence in activities of daily living and addresses functional limitations related to upper limb weakness or sensory deficits. Speech therapy may be beneficial for individuals with GBS who experience dysphagia (difficulty swallowing) or speech impairments due to facial muscle weakness.
Patient Education: Patient education is a cornerstone of GBS management, empowering individuals with knowledge and skills to actively participate in their care and recovery. Key components of patient education include:
- Understanding the condition: Providing information about the nature of GBS, its causes, symptoms, and prognosis can help patients and their families make informed decisions about treatment and self-management strategies.
- Recognition of warning signs: Educating patients about the early signs and symptoms of respiratory distress, autonomic dysfunction, and other complications of GBS enables them to seek prompt medical attention and intervention when necessary.
- Importance of treatment adherence: Emphasizing the importance of adherence to prescribed medications and therapies, such as IVIG or plasma exchange, can optimize treatment outcomes and facilitate recovery.
- Self-care and symptom management: Educating patients about self-care strategies, such as maintaining adequate nutrition, practicing proper body positioning to prevent pressure ulcers, and managing pain and discomfort, can enhance comfort and well-being during the recovery process.
- Rehabilitation and goal-setting: Encouraging patients to actively engage in rehabilitation activities and set realistic goals for functional recovery promotes motivation and participation in the rehabilitation process.
- Psychosocial support: Providing information about available support services, such as support groups, counseling, and community resources, can help address psychosocial needs and enhance coping mechanisms for patients and their families.
Overall, patient education plays a pivotal role in GBS management, fostering collaboration between healthcare providers and patients and empowering individuals to actively participate in their care and recovery journey. By equipping patients with the knowledge and resources they need, healthcare providers can facilitate optimal outcomes and improve the overall quality of life for individuals affected by GBS. (Nursing Paper Example on Guillain-Barré Syndrome: Understanding a Neurological Disorder)
Conclusion
Guillain-Barré Syndrome (GBS) is a complex neurological disorder characterized by immune-mediated peripheral nerve damage, leading to muscle weakness and potential paralysis. Through an exploration of its causes, signs, symptoms, etiology, pathophysiology, DSM-5 diagnosis, treatment regimens, patient education, and implications, we gain a deeper understanding of this condition. By breaking down the causes into infections, vaccinations, and other potential triggers, we acknowledge the multifactorial nature of GBS. Understanding the diverse signs and symptoms, from ascending weakness to autonomic dysfunction, aids in early recognition and intervention. Exploring the etiology highlights the intricate interplay between genetic predisposition, environmental triggers, and immune dysregulation. Examining the pathophysiology uncovers the immune-mediated mechanisms underlying nerve damage in GBS. Considering the DSM-5 diagnosis criteria, treatment regimens, and patient education, we emphasize the importance of a comprehensive approach to managing GBS. Through continued research and holistic care, we strive to improve outcomes and quality of life for individuals living with GBS. (Nursing Paper Example on Guillain-Barré Syndrome: Understanding a Neurological Disorder)



