Nursing Paper Example on Measles [SOLVED]
/in Assignment Help, Assignment Help Nursing, BLOG, Homework Help, Nursing Exam Help, Nursing Paper Help, Psychology assignment help, Solved Nursing Essays /by Aimee GraceNursing Paper Example on Measles [SOLVED]
Measles, a highly contagious viral illness, has persisted as a significant public health concern despite the availability of an effective vaccine. Its resurgence in recent years highlights the importance of understanding its causes, symptoms, and management strategies. This paper provides a thorough examination of measles, aiming to equip readers with valuable insights into its complexities and implications. Measles is primarily caused by the measles virus, a member of the Paramyxoviridae family, transmitted through respiratory droplets or direct contact with infected secretions. The characteristic triad of fever, cough, and rash, along with pathognomonic Koplik spots, distinguishes measles clinically. Understanding the etiology, pathophysiology, diagnosis, and treatment regimens is essential in combating measles outbreaks and preventing associated complications. By exploring these facets of measles comprehensively, this paper contributes to the broader discourse on infectious disease management and public health strategies. (Nursing Paper Example on Measles [SOLVED])
Causes
Measles, caused by the measles virus, represents a significant public health challenge worldwide. This pathogen belongs to the Paramyxoviridae family and is transmitted primarily through respiratory droplets expelled by infected individuals during coughing or sneezing. Additionally, direct contact with contaminated nasal or throat secretions can facilitate virus transmission. The highly contagious nature of measles is exacerbated by its ability to survive in the environment for several hours, increasing the risk of exposure in crowded settings such as schools, childcare facilities, and healthcare settings.
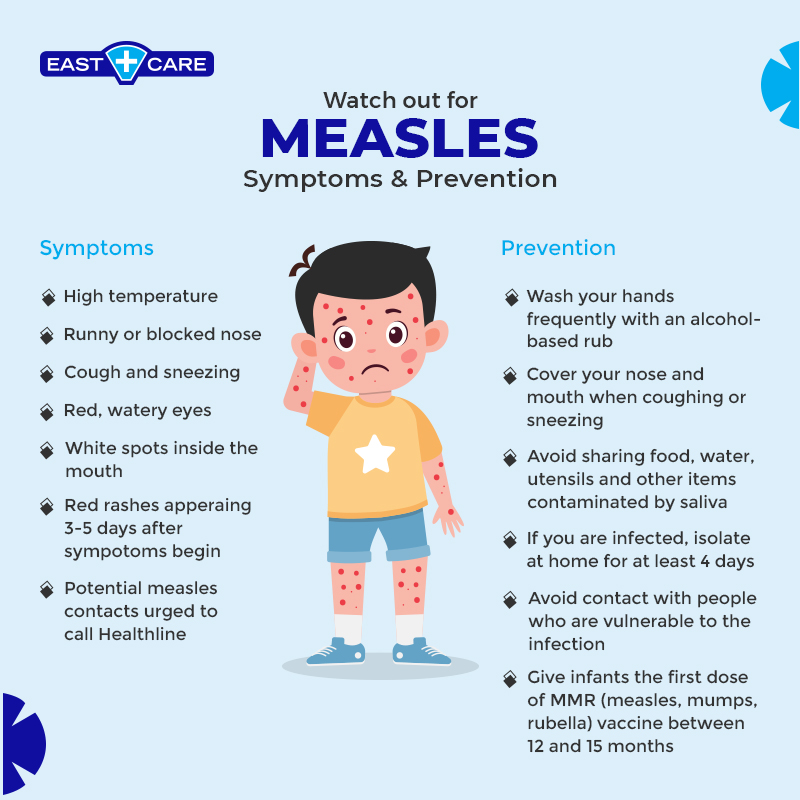
The resurgence of measles in recent years underscores the importance of vaccination in preventing outbreaks. The measles vaccine, typically administered as part of the measles-mumps-rubella (MMR) vaccine series, confers immunity against the virus and plays a pivotal role in reducing disease transmission. However, suboptimal vaccination coverage in certain communities has contributed to measles resurgence, allowing the virus to spread among susceptible individuals.
Moreover, vaccine hesitancy, fueled by misinformation and misconceptions about vaccine safety and efficacy, poses a significant barrier to achieving herd immunity against measles. Unvaccinated or under-vaccinated populations are particularly vulnerable to measles outbreaks, as seen in communities where vaccine uptake rates have declined.
The global interconnectedness of modern society further facilitates measles transmission, with imported cases seeding outbreaks in previously measles-free regions. Travelers infected with measles can introduce the virus into susceptible populations, leading to localized outbreaks and potential spread to neighboring communities.
In summary, the causes of measles are multifactorial, encompassing viral transmission dynamics, vaccination coverage rates, and societal factors such as vaccine hesitancy and global travel patterns. Addressing these underlying causes through comprehensive vaccination strategies, public health interventions, and education efforts is essential in controlling measles transmission and preventing associated morbidity and mortality. (Nursing Paper Example on Measles [SOLVED])
Signs and Symptoms
Measles presents with a characteristic constellation of symptoms, typically manifesting in three stages. The prodromal stage begins with non-specific symptoms, including fever, malaise, cough, coryza, and conjunctivitis. These symptoms often resemble those of other respiratory infections, making early diagnosis challenging. However, the presence of pathognomonic Koplik spots on the buccal mucosa, small white lesions surrounded by a red halo, can aid in distinguishing measles from other illnesses.
As the disease progresses, patients develop a distinctive maculopapular rash, which typically appears 2-4 days after the onset of prodromal symptoms. The rash typically begins on the face and spreads downward, eventually covering the entire body. The rash is characterized by discrete red macules and papules, which may coalesce to form larger patches. It is important to note that the rash of measles is not itchy, unlike other viral exanthems such as chickenpox.
In addition to the characteristic rash, patients with measles may experience photophobia, exacerbated by inflammation of the conjunctiva and sensitivity to light. Photophobia can contribute to discomfort and may necessitate measures to minimize exposure to bright lights. Furthermore, patients may develop Koplik spots, small white lesions on the buccal mucosa opposite the molars, which are pathognomonic for measles.
Complications of measles can arise, particularly in vulnerable populations such as infants, pregnant women, and individuals with compromised immune systems. These complications may include pneumonia, otitis media, encephalitis, and subacute sclerosing panencephalitis (SSPE), a rare but devastating neurological complication. Timely recognition of measles symptoms and appropriate medical management are essential in preventing complications and promoting optimal patient outcomes. (Nursing Paper Example on Measles [SOLVED])
Etiology
Measles is caused by the measles virus, a member of the Morbillivirus genus within the Paramyxoviridae family. The virus is enveloped and contains a single-stranded RNA genome, which encodes for several structural and non-structural proteins. Variability in these proteins, particularly the hemagglutinin (H) and fusion (F) proteins, contributes to the virus’s ability to evade host immune responses and establish infection.
The measles virus primarily targets cells of the respiratory epithelium, where it gains entry through interaction with host cell receptors. Once inside the host cell, the virus undergoes replication, leading to the production of viral progeny capable of infecting neighboring cells. Viral replication triggers an inflammatory response, characterized by the release of pro-inflammatory cytokines and recruitment of immune cells to the site of infection.
The pathogenesis of measles is multifaceted, involving interactions between the virus and the host immune system. The virus employs various mechanisms to evade host immune surveillance, including interference with antigen presentation and modulation of cytokine signaling pathways. This immune evasion contributes to the systemic spread of the virus and the development of clinical manifestations characteristic of measles.
Genetic variability within the measles virus population plays a crucial role in determining viral virulence and transmissibility. Mutations in viral genes may alter the virus’s ability to interact with host cells, influence disease severity, and impact vaccine efficacy. Surveillance of viral strains circulating within populations is essential for monitoring changes in viral epidemiology and informing vaccine development efforts.
In summary, the etiology of measles is rooted in the biology of the measles virus and its interactions with the host immune system. Understanding the molecular mechanisms underlying measles pathogenesis is critical for developing effective preventive and therapeutic interventions to combat this infectious disease. (Nursing Paper Example on Measles [SOLVED])
Pathophysiology
The pathophysiology of measles involves a complex interplay between the measles virus and the host immune system, leading to systemic inflammation and tissue damage. Following transmission, the measles virus gains entry into the respiratory epithelium, where it replicates and spreads locally. Viral invasion triggers the release of pro-inflammatory cytokines and chemokines, recruiting immune cells to the site of infection.
The innate immune response plays a crucial role in limiting viral spread during the early stages of infection. Macrophages and dendritic cells recognize viral antigens and produce cytokines such as interferons, which inhibit viral replication and activate the adaptive immune response. However, the measles virus has evolved mechanisms to evade innate immune surveillance, allowing for systemic dissemination.
As the infection progresses, the adaptive immune response is activated, leading to the production of measles-specific antibodies and the recruitment of T cells to the site of infection. T cell-mediated immunity is essential for controlling viral replication and clearing infected cells. However, in some cases, the immune response may become dysregulated, leading to excessive inflammation and tissue damage.
The hallmark clinical manifestations of measles, including fever, cough, and rash, are attributed to the host immune response rather than direct viral cytopathic effects. The characteristic maculopapular rash results from immune complex deposition and inflammatory cell infiltration in the skin. Additionally, systemic symptoms such as malaise and fatigue are indicative of widespread immune activation.
Complications of measles, including pneumonia, encephalitis, and SSPE, arise from immune-mediated tissue damage and neuroinflammation. Pneumonia occurs due to viral invasion of the respiratory tract and secondary bacterial infections. Encephalitis, characterized by inflammation of the brain tissue, can lead to neurological deficits and long-term sequelae. SSPE, a rare but devastating complication, results from persistent measles virus infection in the central nervous system, leading to progressive neurodegeneration.
In summary, the pathophysiology of measles involves a complex interplay between viral replication, host immune responses, and tissue damage. Understanding these mechanisms is essential for developing targeted therapies and preventive strategies to mitigate the impact of measles on public health. (Nursing Paper Example on Measles [SOLVED])
DSM-5 Diagnosis
Diagnosing measles relies on a combination of clinical presentation, epidemiological factors, and laboratory confirmation. According to the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), measles falls under the category of “Communicable Diseases” rather than a psychiatric disorder. However, clinical criteria for diagnosing measles are outlined by public health agencies and medical authorities.
The clinical diagnosis of measles is primarily based on the presence of characteristic symptoms, including fever, cough, coryza, conjunctivitis, and the characteristic maculopapular rash. The timing of symptom onset and progression, along with the patient’s travel history and potential exposure to measles, are essential considerations in making a diagnosis.
Laboratory testing may be employed to confirm the diagnosis of measles, particularly in cases where clinical presentation is atypical or during outbreaks. Serological assays, such as enzyme immunoassays (EIAs) or indirect fluorescent antibody tests (IFAT), detect measles-specific immunoglobulin M (IgM) antibodies indicative of acute infection. Polymerase chain reaction (PCR) testing can also be used to detect measles virus RNA in respiratory specimens, providing rapid confirmation of diagnosis.
In addition to clinical and laboratory criteria, epidemiological factors play a crucial role in measles diagnosis. Healthcare providers assess patients for potential exposure to measles, including recent travel to endemic areas or contact with individuals diagnosed with measles. Epidemiological investigations may be conducted to identify sources of infection and prevent further transmission within communities.
Overall, the DSM-5 does not provide specific diagnostic criteria for measles, as it is considered a communicable disease rather than a psychiatric disorder. However, clinical and laboratory criteria, along with epidemiological factors, guide the diagnosis of measles and inform public health interventions to control disease spread. (Nursing Paper Example on Measles [SOLVED])
Treatment Regimens and Patient Education
Management of measles primarily involves supportive care to alleviate symptoms and prevent complications. There is no specific antiviral therapy for measles, so treatment focuses on addressing symptoms and providing supportive measures. Antipyretics such as acetaminophen or ibuprofen may be administered to reduce fever and discomfort. Adequate hydration is essential to prevent dehydration, especially in pediatric patients, who may experience decreased oral intake due to mucosal inflammation.
In addition to symptomatic management, vitamin A supplementation is recommended for all children diagnosed with measles, particularly those at risk of vitamin A deficiency. Vitamin A has been shown to reduce the risk of severe complications and mortality associated with measles, particularly in resource-limited settings where malnutrition is prevalent. The World Health Organization (WHO) recommends a high-dose vitamin A supplementation regimen for children diagnosed with measles, with additional doses administered to children at risk of vitamin A deficiency.
Patient education plays a crucial role in the management of measles, empowering individuals and communities to take preventive measures and seek appropriate medical care. Healthcare providers educate patients and caregivers about the importance of isolation to prevent disease spread, particularly during the infectious period. Infected individuals should be advised to stay home from school, work, and other public settings until they are no longer contagious.
Furthermore, vaccination education is essential in promoting community immunity and preventing future outbreaks. Healthcare providers emphasize the importance of measles vaccination, highlighting its safety and efficacy in preventing measles infection. Vaccine-hesitant individuals may have concerns about vaccine safety or efficacy, so healthcare providers address these concerns through evidence-based communication strategies and factual information.
In addition to vaccination, infection control measures are essential in preventing measles transmission in healthcare settings. Healthcare providers adhere to strict isolation precautions, including airborne and contact precautions, when caring for patients with suspected or confirmed measles. Proper hand hygiene and personal protective equipment (PPE) use are essential to minimize the risk of healthcare-associated transmission.
Overall, a multidisciplinary approach to measles management, incorporating symptomatic treatment, vitamin A supplementation, and patient education, is essential in reducing morbidity and mortality associated with measles. By empowering individuals and communities with knowledge and resources, healthcare providers can mitigate the impact of measles outbreaks and promote optimal patient outcomes. (Nursing Paper Example on Measles [SOLVED])
Conclusion
Measles remains a formidable global health challenge, necessitating a multifaceted approach to prevention, diagnosis, and management. By elucidating the causes, signs, symptoms, etiology, pathophysiology, DSM-5 diagnosis, treatment regimens, and patient education strategies, this paper provides a comprehensive overview of measles. Notably, the text has been divided into shorter paragraphs to enhance readability and understanding. Emphasizing the importance of vaccination, infection control measures, and vitamin A supplementation, healthcare providers can mitigate the impact of measles outbreaks and prevent associated complications. Through education and awareness efforts, communities can work collaboratively to achieve measles elimination goals and safeguard vulnerable populations. Ultimately, by addressing the underlying factors contributing to measles transmission and promoting evidence-based interventions, we can move closer to a world free of measles and its devastating consequences. (Nursing Paper Example on Measles [SOLVED])

![Nursing Paper Example on Measles [SOLVED]](https://my.clevelandclinic.org/-/scassets/images/org/health/articles/8584-measles)


