Nursing Paper Example on Pulmonary Embolism
Nursing Paper Example on Pulmonary Embolism
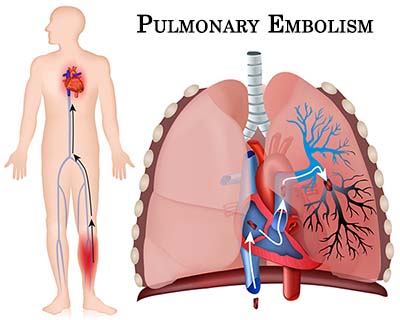
Pulmonary embolism (PE) is a serious and potentially life-threatening condition that occurs when a blood clot, often originating from the deep veins in the legs (deep vein thrombosis or DVT), travels through the bloodstream and becomes lodged in the pulmonary arteries. This blockage can impede blood flow to the lungs, causing a reduction in oxygen levels in the body and damage to lung tissue. PE is a medical emergency, as it can lead to severe complications such as heart failure or death if not treated promptly.
Causes and Risk Factors
The primary cause of PE is the formation of a blood clot, or thrombus, that typically originates from the deep veins in the legs or pelvis. Once dislodged, this clot can travel through the venous system and become trapped in the pulmonary arteries. Several factors increase the risk of clot formation, including:
- Prolonged immobility: Extended periods of inactivity, such as during long flights, hospitalization, or bed rest, can slow blood circulation and increase the likelihood of clot formation.
- Surgery: Major surgeries, particularly orthopedic or abdominal procedures, can increase the risk of clot formation due to trauma to blood vessels and prolonged immobilization.
- Cancer: Some cancers, particularly those affecting the lungs, pancreas, and brain, are associated with a higher risk of clot formation.
- Pregnancy: Hormonal changes and increased pressure on pelvic veins during pregnancy increase the risk of clotting.
- Smoking: Smoking damages blood vessels and promotes clot formation.
- Obesity: Being overweight increases the strain on the heart and circulatory system, making clot formation more likely.
Signs and Symptoms
The presentation of PE can vary depending on the size of the clot and the extent of blockage in the pulmonary arteries. Common symptoms include:
- Sudden shortness of breath: Difficulty breathing is one of the most common and immediate symptoms of PE.
- Chest pain: The pain is often sharp and may worsen with deep breaths or coughing.
- Coughing: Some individuals with PE may cough up blood (hemoptysis).
- Rapid heart rate: An abnormally fast heart rate (tachycardia) may occur as the heart tries to compensate for reduced oxygen levels.
- Fainting or dizziness: Severe PE can lead to lightheadedness or syncope (fainting) due to reduced oxygen supply to the brain.
These symptoms can overlap with other conditions, such as heart attack or pneumonia, making timely diagnosis essential.
Pathophysiology
Pulmonary embolism occurs when a thrombus dislodges and travels to the pulmonary arteries, causing partial or complete obstruction. The blockage reduces or halts the flow of blood to lung tissue, which can lead to ischemia and lung infarction. The decreased oxygen exchange in the lungs results in hypoxemia, which can lead to tissue damage throughout the body, including the heart and brain. Large emboli can cause sudden increases in pulmonary artery pressure, leading to acute right ventricular failure, while smaller emboli may lead to gradual damage through recurrent episodes.
The Virchow’s triad describes the three main factors that contribute to clot formation: venous stasis, endothelial injury, and hypercoagulability. These factors play a key role in the development of PE, particularly in patients with prolonged immobility or underlying clotting disorders.
Types of Pulmonary Embolism
PE can be classified based on the size and location of the clot within the pulmonary arteries:
- Massive PE: A large clot that obstructs the main pulmonary artery or branches, leading to severe symptoms, shock, or sudden death.
- Submassive PE: Involves partial blockage of the pulmonary arteries, causing moderate symptoms and risk of right heart strain.
- Segmental or subsegmental PE: Involves smaller clots in the peripheral branches of the pulmonary arteries, causing milder symptoms and a lower risk of mortality.
Diagnosis
Diagnosing PE involves a combination of clinical assessment, imaging tests, and laboratory findings. Physicians may use the following tools:
- D-dimer test: Elevated D-dimer levels suggest the presence of blood clots, although it is a non-specific marker.
- Computed tomography pulmonary angiography (CTPA): A contrast-enhanced CT scan is the gold standard for diagnosing PE. It allows for the visualization of blood clots in the pulmonary arteries.
- Ventilation-perfusion (V/Q) scan: This nuclear medicine scan measures the airflow and blood flow in the lungs, helping to identify mismatches caused by clots.
- Echocardiography: This imaging technique is useful for assessing the strain on the right ventricle, particularly in cases of massive PE.
- Ultrasound of the legs: A duplex ultrasound may be used to detect DVT in the legs, the most common source of clots that cause PE.
(Nursing Paper Example on Pulmonary Embolism)
Treatment Regimens
The treatment of PE focuses on preventing further clot formation, breaking up existing clots, and stabilizing the patient. The main approaches include:
- Anticoagulants: These blood thinners, such as heparin, warfarin, and newer direct oral anticoagulants (DOACs), prevent the formation of new clots and allow the body to break down the existing clot.
- Thrombolytics: In life-threatening cases or massive PE, clot-busting drugs like alteplase may be administered to dissolve large clots rapidly.
- Surgical interventions: For patients who cannot take anticoagulants or fail to respond to medication, a surgical procedure such as embolectomy (removal of the clot) may be necessary.
- Inferior vena cava (IVC) filter: In patients at high risk for recurrent PE, an IVC filter may be inserted to trap clots before they reach the lungs.
Long-term management involves continued use of anticoagulants for several months or even lifelong treatment, depending on the underlying cause of the clot.
Patient Education and Prevention
Patients recovering from PE must understand the importance of adherence to prescribed anticoagulant therapy to prevent future embolic events. Education should focus on recognizing the early signs of DVT and PE, such as leg swelling, warmth, and pain, and the need for immediate medical attention if symptoms occur. Lifestyle modifications that reduce the risk of clot formation are critical, such as:
- Staying active: Regular physical activity helps improve blood circulation, particularly for those who are sedentary or recovering from surgery.
- Hydration: Adequate fluid intake prevents blood thickening, which can contribute to clot formation.
- Compression stockings: Wearing compression stockings can improve circulation and reduce the risk of DVT, especially for those who are immobile or have a history of clotting.
Complications
Complications from PE can be severe, particularly in cases where treatment is delayed or inadequate. Some of the most common complications include:
- Pulmonary hypertension: Chronic clots in the pulmonary arteries can lead to elevated blood pressure in the lungs, causing long-term strain on the heart.
- Right ventricular dysfunction: Large or recurrent clots can cause the right side of the heart to work harder to pump blood, potentially leading to heart failure.
- Post-thrombotic syndrome: Following PE, some patients may experience chronic leg pain, swelling, and ulcers due to damage to the veins from DVT.
(Nursing Paper Example on Pulmonary Embolism)
Conclusion
Pulmonary embolism is a life-threatening condition that requires prompt diagnosis and treatment. Recognizing the causes, risk factors, and early signs of PE is crucial for preventing severe complications. Anticoagulant therapy remains the cornerstone of treatment, and lifestyle modifications can help reduce the risk of recurrent clots. Ongoing patient education and adherence to treatment are essential for long-term management. By understanding the complexity of PE and its impact on the cardiovascular system, healthcare providers can effectively manage and reduce the burden of this potentially fatal condition.
References
- Centers for Disease Control and Prevention (CDC). Pulmonary Embolism. https://www.cdc.gov/ncbddd/dvt/pulmonary-embolism.html
- Mayo Clinic. Pulmonary embolism. https://www.mayoclinic.org/diseases-conditions/pulmonary-embolism/symptoms-causes/syc-20354647
- Konstantinides, S. V., et al. (2020). 2019 ESC Guidelines for the diagnosis and management of acute pulmonary embolism. European Heart Journal, 41(4), 543-603. https://academic.oup.com/eurheartj/article/41/4/543/5543761
- Beckman, M. G., et al. (2010). Venous thromboembolism: A public health concern. American Journal of Preventive Medicine, 38(4), S495-S501. https://doi.org/10.1016/j.amepre.2009.12.017



