Nursing Paper Example on Sepsis
Nursing Paper Example on Sepsis
Sepsis is a life-threatening condition triggered by a dysregulated immune response to infection, leading to widespread inflammation and potential organ failure. It poses significant health challenges globally, with millions of cases reported each year. Recognizing, diagnosing, and managing sepsis promptly is essential to improving survival rates and reducing complications.
Causes of Sepsis
Sepsis is primarily caused by bacterial infections, though fungal, viral, and parasitic pathogens can also lead to sepsis. Common infections leading to sepsis include:
- Respiratory Infections: Pneumonia is among the most frequent origins of sepsis, especially in the elderly and immunocompromised.
- Urinary Tract Infections: Particularly in elderly populations and those with underlying conditions, urinary tract infections can lead to sepsis.
- Skin Infections: Infections from wounds, cellulitis, and pressure ulcers can also result in sepsis.
- Abdominal Infections: Appendicitis, peritonitis, and intra-abdominal abscesses are also significant causes (Singer et al., 2016).
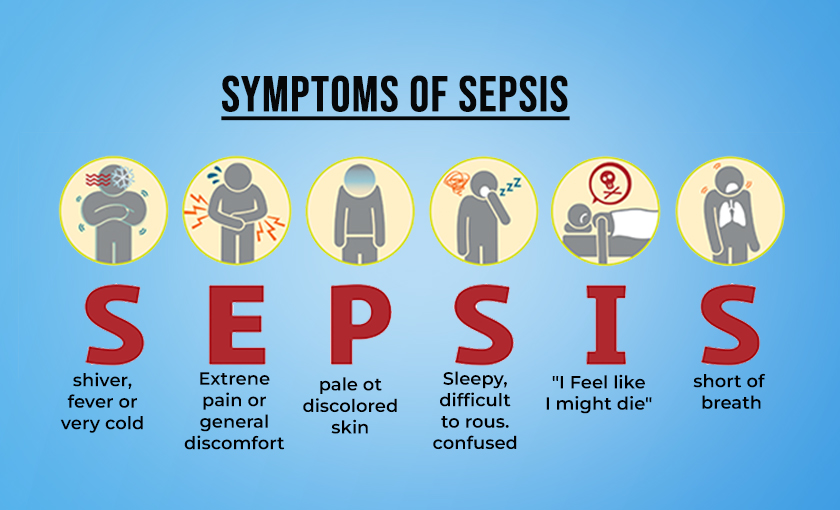
Signs and Symptoms
Sepsis symptoms can progress rapidly, requiring timely recognition. Symptoms include:
- Fever, chills, and sweating: Body temperature often rises due to infection but may drop in severe cases.
- Rapid heartbeat and breathing: An elevated heart rate and respiratory rate are early indicators.
- Altered mental status: Confusion or lethargy can signify reduced oxygen flow to the brain.
- Hypotension: Low blood pressure is often a hallmark of sepsis, especially in septic shock cases.
- Organ dysfunction: As sepsis progresses, it can lead to dysfunction in organs such as the kidneys, liver, and lungs, potentially progressing to multi-organ failure if untreated.
These symptoms often escalate, requiring swift intervention to prevent organ damage and death (Vincent et al., 2019).
Etiology
The primary cause of sepsis is an exaggerated immune response to infection, where immune cells release excessive inflammatory mediators, leading to systemic inflammation. Key factors that contribute to sepsis include:
- Age: Older adults and infants are at higher risk.
- Comorbidities: Diabetes, chronic kidney disease, and other conditions predispose individuals to severe infections.
- Immunosuppression: Individuals with compromised immune systems, including those undergoing chemotherapy or those with HIV, are at elevated risk.
- Invasive Devices: Catheters, ventilators, and other devices increase infection risk, especially in hospital settings.
Genetic factors can also play a role, as certain genotypes may make individuals more susceptible to sepsis (Rello et al., 2018).
Pathophysiology
Sepsis involves a complex chain reaction of immune responses and vascular changes:
- Inflammatory Cascade: The immune system releases cytokines and pro-inflammatory mediators in response to pathogens, leading to vasodilation, increased capillary permeability, and coagulation abnormalities.
- Endothelial Dysfunction: The inner lining of blood vessels becomes compromised, resulting in fluid leakage, tissue edema, and impaired oxygen transport.
- Coagulation Cascade Activation: Sepsis triggers widespread clot formation, potentially leading to disseminated intravascular coagulation, which can cause tissue ischemia and multi-organ failure.
- Organ Dysfunction: Due to reduced blood flow and oxygen delivery, organs such as the kidneys, liver, lungs, and brain begin to malfunction, worsening the condition (Hotchkiss et al., 2016).
Diagnosis
Diagnosis of sepsis is challenging and relies on a combination of clinical evaluation and laboratory tests:
- SIRS Criteria: Initially, the Systemic Inflammatory Response Syndrome (SIRS) criteria were used to identify sepsis by measuring body temperature, heart rate, respiratory rate, and white blood cell count. However, SIRS is less commonly used today.
- SOFA and qSOFA Scores: The Sequential Organ Failure Assessment (SOFA) and its quick version, qSOFA, are used to predict sepsis mortality risk. Key indicators include blood pressure, respiratory rate, and mental status.
- Biomarkers: Blood tests measuring lactate levels, C-reactive protein, procalcitonin, and white blood cell counts help confirm infection and organ dysfunction.
- Blood Cultures and Imaging: Cultures help identify the pathogen, while imaging (X-ray, CT, ultrasound) can locate the infection site.
The use of biomarkers and imaging, along with SOFA scoring, provides a more accurate prognosis of sepsis (Shankar-Hari et al., 2016).
Treatment Regimens
Management of sepsis involves rapid intervention to control infection, stabilize the patient, and support failing organs. Core treatment components include:
- Antibiotic Therapy: Broad-spectrum antibiotics are started immediately and adjusted based on culture results.
- Fluid Resuscitation: Intravenous fluids help restore blood volume and improve blood pressure. Typically, crystalloid solutions are preferred.
- Vasopressors: In cases of persistent hypotension, vasopressors like norepinephrine are used to maintain adequate blood pressure.
- Organ Support: Mechanical ventilation, renal replacement therapy, and other organ-supportive measures are used as necessary.
- Corticosteroids: In severe cases, low-dose corticosteroids may help reduce inflammation and stabilize blood pressure (Rhodes et al., 2017).
Patient Education
Education is essential for prevention and recovery. Key areas for patient education include:
- Infection Prevention: Handwashing, vaccination, and wound care reduce infection risks.
- Early Symptom Recognition: Patients and caregivers should recognize early symptoms and seek immediate medical attention.
- Post-Sepsis Syndrome Awareness: Many survivors experience lasting effects, such as chronic pain, fatigue, and cognitive issues. Patients should be educated about these potential symptoms and encouraged to seek ongoing support.
- Lifestyle Modification: Patients should adopt a healthy lifestyle, including good nutrition, regular physical activity, and avoiding tobacco, to support recovery and prevent future infections (Prescott & Angus, 2018).
Conclusion
Sepsis is a complex, life-threatening condition requiring rapid diagnosis, prompt treatment, and patient education. Understanding the pathophysiology, risk factors, and management strategies is crucial for healthcare professionals. Timely intervention significantly improves outcomes, underscoring the importance of education for both providers and patients.
References
Hotchkiss, R. S., Moldawer, L. L., Opal, S. M., Reinhart, K., Turnbull, I. R., & Vincent, J. L. (2016). Sepsis and septic shock. Nature Reviews Disease Primers, 2(1), 1-21. https://www.nature.com/articles/nrdp201622
Prescott, H. C., & Angus, D. C. (2018). Enhancing recovery from sepsis: A review. JAMA, 319(1), 62-75. https://jamanetwork.com/journals/jama/article-abstract/2666320
Rello, J., Valenzuela-Sánchez, F., Ruiz-Rodriguez, M., & Moyano, S. (2018). Sepsis: A review of advances in management. Advances in Therapy, 34(11), 2393-2411. https://link.springer.com/article/10.1007/s12325-018-0649-3
Rhodes, A., Evans, L. E., Alhazzani, W., Levy, M. M., Antonelli, M., Ferrer, R., … & Dellinger, R. P. (2017). Surviving sepsis campaign: International guidelines for management of sepsis and septic shock. Intensive Care Medicine, 43(3), 304-377. https://link.springer.com/article/10.1007/s00134-017-4683-6
Shankar-Hari, M., Phillips, G. S., Levy, M. L., Seymour, C. W., Liu, V. X., Deutschman, C. S., … & Angus, D. C. (2016). Developing a new definition and assessing new clinical criteria for septic shock: For the Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA, 315(8), 775-787. https://jamanetwork.com/journals/jama/fullarticle/2492881
Singer, M., Deutschman, C. S., Seymour, C. W., Shankar-Hari, M., Annane, D., Bauer, M., … & Angus, D. C. (2016). The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA, 315(8), 801-810. https://jamanetwork.com/journals/jama/fullarticle/2492881



