Nursing Paper Example on Synovitis
Nursing Paper Example on Synovitis
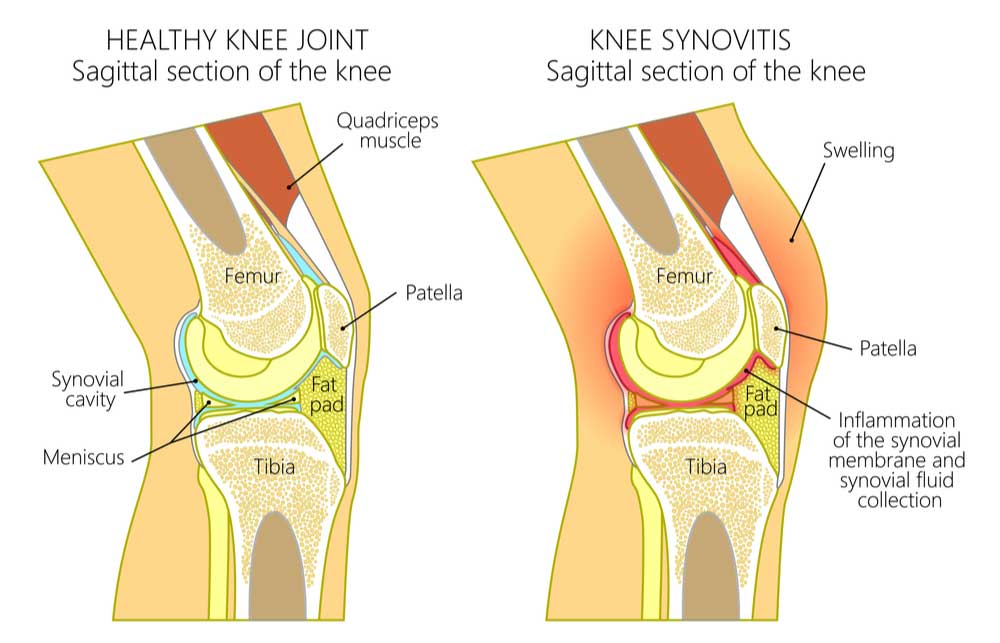
Synovitis is an inflammatory condition affecting the synovial membrane, which lines joint cavities. The inflammation leads to pain, swelling, and stiffness in the affected joints. It commonly occurs in association with various forms of arthritis but can also result from injury, infection, or other diseases. A thorough understanding of synovitis includes exploring its causes, symptoms, diagnostic methods, treatment options, complications, and preventive measures.
Causes and Risk Factors
Primary Causes
Synovitis results from inflammation in the synovial membrane. This inflammation can stem from:
- Rheumatoid Arthritis: The most common cause of chronic synovitis, resulting in autoimmunity where the body mistakenly attacks the synovium.
- Trauma: Joint injuries can trigger inflammation as the body attempts to repair itself.
- Infections: Bacterial or viral infections can lead to septic synovitis, where the joint becomes infected and inflamed.
- Gout and Pseudogout: The deposition of uric acid or calcium pyrophosphate crystals within the joints can trigger synovitis.
- Other Systemic Diseases: Conditions like lupus and psoriatic arthritis can also contribute to synovial inflammation (Smolen et al., 2018).
(Nursing Paper Example on Synovitis)
Risk Factors
Several factors increase the likelihood of developing synovitis:
- Age: Synovitis risk increases with age due to the higher likelihood of arthritis.
- Previous Joint Injuries: Injuries from sports or accidents can predispose individuals to synovitis.
- Autoimmune Diseases: A history of autoimmune conditions may heighten the risk.
- Occupational Activities: Jobs involving repetitive joint movement can lead to synovial inflammation over time (McInnes & Schett, 2017).
Signs and Symptoms
Synovitis symptoms vary depending on the severity and underlying cause but typically include:
- Joint Swelling: Visible swelling occurs due to fluid accumulation in the joint.
- Pain: Joints feel sore, especially during movement or pressure.
- Stiffness: Morning stiffness or difficulty moving the joint, which may improve with activity.
- Warmth and Redness: Inflamed joints often feel warm and may have a reddish hue.
- Limited Range of Motion: Due to swelling and pain, the joint’s normal movement may become restricted.
These symptoms are commonly seen in joints such as the knees, elbows, wrists, and ankles. Chronic synovitis can eventually cause damage to the joint and lead to joint deformities if left untreated (Filer, 2018).
Pathophysiology
Synovitis involves an immune response in the synovial membrane. In cases of autoimmune disease, the body mistakenly targets synovial cells, leading to inflammation. The inflammatory process is marked by the accumulation of immune cells like macrophages and T cells, which release pro-inflammatory cytokines such as interleukin-1 (IL-1) and tumor necrosis factor-alpha (TNF-α). These cytokines promote further inflammation, leading to swelling, increased blood flow, and joint damage. Over time, persistent inflammation can cause the thickening of the synovial lining, called pannus formation, which further restricts joint mobility and damages cartilage (McInnes & Schett, 2017).
Diagnosis
Clinical Examination
A healthcare provider typically starts by examining the affected joint for swelling, warmth, and limited motion. Patient history, including recent injuries, infections, or pre-existing autoimmune conditions, is also considered.
Imaging Tests
- Ultrasound: An ultrasound of the joint helps visualize the inflamed synovial membrane and fluid accumulation.
- Magnetic Resonance Imaging (MRI): MRI can provide a detailed image of the joint structure and is particularly useful in identifying synovitis in deep joints.
Laboratory Tests
- Blood Tests: Used to detect markers of inflammation, including C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR), and to test for autoimmune markers like rheumatoid factor (RF) and anti-cyclic citrullinated peptide (anti-CCP) antibodies.
- Joint Aspiration (Arthrocentesis): A sample of synovial fluid is collected and analyzed for signs of infection, crystals, or inflammatory cells (Filer, 2018).
(Nursing Paper Example on Synovitis)
Treatment
Synovitis treatment focuses on reducing inflammation, alleviating pain, and addressing the underlying cause:
- Medication:
- Non-Steroidal Anti-Inflammatory Drugs (NSAIDs): Commonly used to reduce inflammation and relieve pain.
- Corticosteroids: Can be injected directly into the joint for rapid inflammation reduction.
- Disease-Modifying Antirheumatic Drugs (DMARDs): Used for chronic autoimmune-related synovitis, these drugs, including methotrexate, help slow disease progression.
- Biologic Agents: For rheumatoid arthritis-related synovitis, biologics like TNF inhibitors may be used to target specific immune pathways (Smolen et al., 2018).
- Physical Therapy:
- Exercises to maintain joint flexibility and strength can help patients maintain function and prevent stiffness.
- Surgery:
- In severe cases, surgical options like synovectomy (removal of the inflamed synovium) may be considered to relieve pain and prevent further joint damage.
- Lifestyle Modifications:
- Rest and Joint Protection: Reducing stress on affected joints can help manage pain and inflammation.
- Weight Management: For weight-bearing joints, weight loss can reduce joint strain and inflammation.
Timely diagnosis and treatment are essential to prevent the progression of joint damage in synovitis (McInnes & Schett, 2017).
Complications
Untreated or recurrent synovitis can lead to significant complications:
- Chronic Joint Damage: Persistent inflammation can cause cartilage and bone damage, resulting in reduced joint mobility.
- Joint Deformities: Severe cases may lead to structural changes in the joint, impairing function.
- Infection: Synovitis caused by infections, if left untreated, can spread and result in septic arthritis, a serious and potentially life-threatening condition (Filer, 2018).
Prevention
Preventing synovitis involves reducing risk factors and addressing underlying conditions:
- Prompt Treatment of Joint Injuries: Reduces the risk of post-traumatic synovitis.
- Manage Autoimmune Disorders: Early diagnosis and management of autoimmune diseases can help prevent inflammation in the joints.
- Infection Control: Maintaining proper hygiene, treating infections promptly, and avoiding exposure to pathogens can reduce the risk of infectious synovitis.
- Protective Equipment: Individuals with high-impact jobs or those involved in sports should use joint protection to minimize trauma (Smolen et al., 2018).
Conclusion
Synovitis, a condition characterized by synovial membrane inflammation, often coexists with other joint disorders and diseases. From autoimmune origins to traumatic injury, multiple factors can initiate and exacerbate synovitis. Prompt diagnosis through physical exams, imaging, and laboratory tests can significantly improve treatment outcomes. Treatment approaches focus on reducing inflammation, managing symptoms, and addressing underlying causes. Preventing synovitis requires both managing primary risk factors and adopting protective measures, particularly for those prone to joint injuries or autoimmune conditions.
References
Filer, A. (2018). The role of synovitis in the pathophysiology of rheumatoid arthritis. Arthritis Research & Therapy, 20(1), 1-7. https://arthritis-research.biomedcentral.com/articles/10.1186/s13075-018-1533-z
McInnes, I. B., & Schett, G. (2017). Pathogenetic insights from the synovium in autoimmunity and inflammation. Current Opinion in Rheumatology, 29(2), 125-130. https://journals.lww.com/co-rheumatology/Abstract/2017/03000/Pathogenetic_insights_from_the_synovium_in.4.aspx
Smolen, J. S., Aletaha, D., & McInnes, I. B. (2018). Rheumatoid arthritis. The Lancet, 388(10055), 2023-2038. https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(18)31791-5/fulltext



