Nursing Paper Example on Understanding Encephalitis: Causes, Symptoms, Treatment, and Patient Care
Causes
Encephalitis has various causes, spanning infectious and non-infectious origins. Viral infections are predominant culprits, with herpes simplex virus (HSV) and varicella-zoster virus (VZV) being common offenders. These viruses can directly invade the brain, triggering an inflammatory response and leading to encephalitis. Additionally, other viral agents such as enteroviruses, arboviruses (e.g., West Nile virus), and influenza viruses can also induce encephalitis.
Bacterial infections like Lyme disease, caused by Borrelia burgdorferi, can result in neuroborreliosis, leading to encephalitis in some cases. Moreover, certain parasitic infections, such as toxoplasmosis and malaria, can cause encephalitis through indirect mechanisms.
Non-infectious triggers, including autoimmune reactions, can also contribute to encephalitis. Autoimmune encephalitis occurs when the body’s immune system mistakenly attacks healthy brain tissue, leading to inflammation and neurological dysfunction. Conditions like anti-NMDA receptor encephalitis and autoimmune limbic encephalitis exemplify this mechanism.
Environmental factors such as exposure to toxins or chemicals may also precipitate encephalitis. For instance, exposure to heavy metals like lead or mercury can trigger neuroinflammation, potentially leading to encephalitis.
Furthermore, immunocompromised individuals, such as those with HIV/AIDS or undergoing immunosuppressive therapy, are at higher risk of developing encephalitis due to their weakened immune defenses.
Understanding the diverse array of causes underlying encephalitis is crucial for accurate diagnosis and targeted treatment. Differentiating between infectious and non-infectious etiologies guides clinicians in selecting appropriate therapeutic interventions and optimizing patient outcomes. Thus, a comprehensive understanding of encephalitis causes is essential for effective management and improved prognosis.
Signs and Symptoms
Encephalitis manifests through a spectrum of signs and symptoms, often varying in severity and presentation. The hallmark features typically include fever, headache, and altered mental status, which may range from mild confusion to profound disorientation or coma. These cognitive changes often accompany behavioral alterations, including irritability, agitation, or personality changes.
:max_bytes(150000):strip_icc()/VWH-MiraNorian-Encephalitis-4000x2700-d724354b09df4b4a81520987ba5f6b52.png)
Neurological manifestations of encephalitis can encompass a wide array of symptoms, such as seizures, focal neurological deficits, and impaired consciousness. Seizures may manifest as generalized convulsions or focal motor seizures, further complicating the clinical picture.
In some cases, patients may exhibit psychiatric symptoms, including psychosis, hallucinations, or delusions, reflecting the profound impact of encephalitis on brain function. Additionally, movement disorders such as tremors, ataxia, or dyskinesias may arise due to disruption of neural circuits within the basal ganglia or cerebellum.
Furthermore, encephalitis can lead to autonomic dysfunction, presenting as fluctuations in blood pressure, heart rate, or temperature regulation. These autonomic disturbances contribute to the overall clinical complexity of encephalitis and may pose challenges in management.
Children with encephalitis may exhibit distinct symptoms, including irritability, lethargy, poor feeding, or developmental regression. Early recognition of these pediatric-specific signs is critical for prompt diagnosis and intervention.
It is essential to recognize the broad spectrum of signs and symptoms associated with encephalitis, as timely identification facilitates early initiation of appropriate treatment and improves clinical outcomes. Vigilance for subtle neurological changes, particularly in high-risk populations, is paramount for early intervention and preventing potential complications. Thus, a comprehensive understanding of encephalitis symptoms is essential for timely diagnosis and effective management. (Nursing Paper Example on Understanding Encephalitis: Causes, Symptoms, Treatment, and Patient Care)
Etiology
Encephalitis encompasses a diverse etiology, reflecting the multifaceted nature of this neurological disorder. Viral infections stand as predominant etiological factors, with herpes simplex virus (HSV) and varicella-zoster virus (VZV) accounting for a significant proportion of cases. These viruses gain access to the central nervous system (CNS) via neuronal pathways, causing direct neuronal injury and triggering an inflammatory response within the brain.
Other viral agents, including enteroviruses, arboviruses (e.g., West Nile virus), and influenza viruses, can also precipitate encephalitis through various mechanisms. These viruses may disseminate hematogenously or via peripheral nerves, leading to CNS invasion and subsequent neuroinflammation.
Bacterial infections represent another important etiological category, with pathogens such as Borrelia burgdorferi (causing Lyme disease) and Mycobacterium tuberculosis capable of inducing encephalitis. These bacteria may infiltrate the CNS through hematogenous spread or direct extension from adjacent structures, inciting an inflammatory cascade within the brain parenchyma.
Parasitic infections, though less common, can also contribute to encephalitis pathogenesis. Toxoplasma gondii and Plasmodium species (causing malaria) are notable examples, with encephalitis arising secondary to parasitic invasion of the CNS and subsequent inflammatory response.
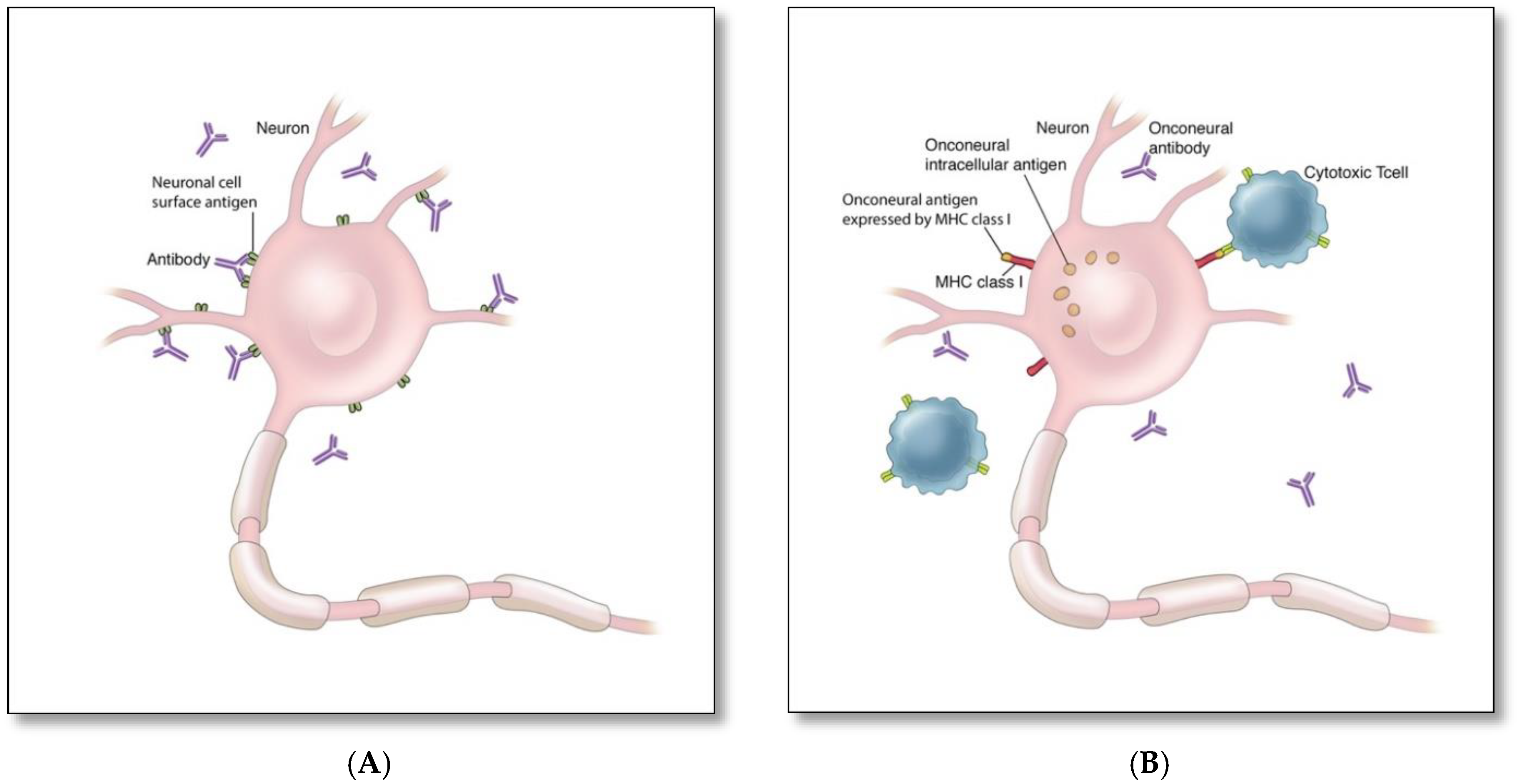
Non-infectious etiologies, particularly autoimmune reactions, are increasingly recognized as significant contributors to encephalitis. Autoimmune encephalitis encompasses a spectrum of disorders characterized by immune-mediated attacks on neuronal antigens, leading to neuroinflammation and neurological dysfunction.
Furthermore, environmental factors such as exposure to toxins or chemicals may precipitate encephalitis by eliciting neuroinflammatory responses within the brain. Understanding the diverse etiological factors underlying encephalitis is crucial for accurate diagnosis and targeted therapeutic interventions, ultimately improving patient outcomes and guiding preventive strategies. (Nursing Paper Example on Understanding Encephalitis: Causes, Symptoms, Treatment, and Patient Care)
Pathophysiology
The pathophysiology of encephalitis involves a complex interplay of inflammatory cascades, immune responses, and neuronal dysfunction, culminating in neurological impairment. Viral encephalitis typically begins with viral invasion of the central nervous system (CNS), facilitated by hematogenous dissemination or neuronal spread from peripheral sites of infection. Upon entering the CNS, viruses target neurons, glial cells, and endothelial cells, initiating a robust immune response characterized by cytokine release and activation of resident immune cells.
This inflammatory milieu triggers endothelial cell activation and disruption of the blood-brain barrier (BBB), allowing infiltration of immune cells into the brain parenchyma. Activated microglia and infiltrating macrophages release pro-inflammatory mediators, exacerbating neuroinflammation and promoting neuronal injury.
In addition to direct viral-induced damage, immune-mediated mechanisms contribute to neuronal dysfunction in encephalitis. Autoimmune encephalitis, for instance, results from antibodies targeting neuronal antigens, leading to synaptic dysfunction, neuronal excitotoxicity, and impaired neurotransmission.
The ensuing neuronal injury and inflammation disrupt neural circuits and neurotransmitter pathways, manifesting clinically as altered mental status, seizures, and focal neurological deficits. Moreover, disruption of the BBB facilitates the entry of neurotoxic substances and exacerbates neuroinflammation, further exacerbating neuronal injury.
The pathophysiological processes underlying encephalitis are dynamic and multifactorial, involving a delicate balance between viral replication, immune responses, and neuronal damage. Understanding these mechanisms is crucial for developing targeted therapeutic strategies aimed at mitigating neuroinflammation, preserving neuronal function, and optimizing patient outcomes. Further research into the pathophysiology of encephalitis is warranted to unravel its complexities and identify novel therapeutic targets for intervention. (Nursing Paper Example on Understanding Encephalitis: Causes, Symptoms, Treatment, and Patient Care)
DSM-5 Diagnosis
Diagnosing encephalitis entails a comprehensive evaluation based on clinical presentation, laboratory findings, and neuroimaging studies, as outlined in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5). The DSM-5 provides criteria for diagnosing neurocognitive disorders, including those resulting from infectious or inflammatory etiologies such as encephalitis.
The DSM-5 criteria emphasize the presence of significant cognitive decline from a previous level of functioning, which may manifest as impaired memory, executive function, attention, or language skills. Additionally, individuals with encephalitis may exhibit disturbances in consciousness, orientation, perception, or behavior, reflecting the multifaceted nature of the disorder.
Laboratory investigations play a crucial role in confirming the diagnosis of encephalitis. Cerebrospinal fluid (CSF) analysis reveals lymphocytic pleocytosis, elevated protein levels, and sometimes the presence of specific pathogens or antibodies indicative of viral or autoimmune etiologies. Serological tests for viral antibodies and polymerase chain reaction (PCR) assays can identify viral pathogens circulating in the CNS.
Neuroimaging studies, particularly magnetic resonance imaging (MRI) of the brain, may demonstrate characteristic findings such as focal or diffuse signal abnormalities in the affected brain regions. These imaging findings complement clinical and laboratory assessments, aiding in confirming the diagnosis of encephalitis and guiding treatment decisions.
The DSM-5 diagnosis of encephalitis underscores the importance of a multidisciplinary approach involving neurologists, infectious disease specialists, and psychiatrists. By integrating clinical, laboratory, and imaging data, healthcare professionals can accurately diagnose encephalitis and initiate timely interventions to optimize patient outcomes. Moreover, adherence to DSM-5 criteria ensures consistency and precision in diagnosing encephalitis across diverse clinical settings, facilitating effective management and support for affected individuals. (Nursing Paper Example on Understanding Encephalitis: Causes, Symptoms, Treatment, and Patient Care)
Treatment Regimens and Patient Education
Treatment of encephalitis necessitates a multifaceted approach aimed at addressing the underlying cause, managing symptoms, and preventing complications. Antiviral therapy is the mainstay of treatment for viral encephalitis, targeting specific viral pathogens such as herpes simplex virus (HSV) or varicella-zoster virus (VZV). Intravenous administration of antiviral medications like acyclovir or ganciclovir is initiated promptly upon suspicion of viral encephalitis to mitigate viral replication and reduce neuronal damage.
In cases of bacterial encephalitis, antibiotic therapy targeting the causative pathogen is imperative. Prompt initiation of antibiotics like ceftriaxone or penicillin G is crucial to combat bacterial invasion of the central nervous system (CNS) and prevent systemic complications.
In autoimmune encephalitis, immunomodulatory therapy aims to suppress the aberrant immune response directed against neuronal antigens. Treatment may involve corticosteroids, intravenous immunoglobulin (IVIG), or immunosuppressive agents like rituximab or cyclophosphamide to attenuate neuroinflammation and preserve neuronal function.
Supportive care plays a pivotal role in managing complications and promoting recovery in patients with encephalitis. This includes close monitoring of vital signs, maintenance of adequate hydration, seizure management, and addressing nutritional needs. In severe cases with neurological sequelae, rehabilitation therapy may be necessary to optimize functional outcomes and enhance quality of life.
Patient education is integral to the management of encephalitis, empowering individuals and their caregivers to navigate the challenges associated with the condition. Patients should be educated about the importance of adhering to prescribed medications, attending follow-up appointments, and recognizing warning signs of disease progression or relapse. Furthermore, patients and caregivers should receive guidance on strategies to optimize brain health, including adequate rest, nutrition, and cognitive stimulation.
Moreover, raising awareness about encephalitis within the community is crucial to promoting early recognition and timely intervention. Educational initiatives aimed at healthcare providers, schools, and the general public can facilitate prompt referral to specialized care centers and improve outcomes for individuals affected by encephalitis.
The treatment of encephalitis involves a comprehensive approach encompassing specific antiviral or antibiotic therapy, immunomodulatory interventions, and supportive care measures. Patient education is paramount in empowering individuals and caregivers to actively participate in disease management and promote optimal outcomes. By addressing both the medical and educational aspects of encephalitis, healthcare providers can enhance the quality of care and support for affected individuals and their families. (Nursing Paper Example on Understanding Encephalitis: Causes, Symptoms, Treatment, and Patient Care)




