Nursing Paper Example on Understanding Schizophrenia: A Comprehensive Overview
Nursing Paper Example on Understanding Schizophrenia: A Comprehensive Overview
Causes
Schizophrenia is a multifaceted disorder with a complex interplay of genetic, environmental, and neurobiological factors contributing to its development. Genetic predisposition is a significant component, with studies indicating a higher risk among individuals with family members affected by the disorder. Specific genes related to neurotransmitter regulation and brain development have been identified as potential contributors to schizophrenia susceptibility.
Environmental factors also play a role in the onset of schizophrenia. Prenatal exposure to infections, maternal stress during pregnancy, and birth complications have been associated with an increased risk of developing the disorder. Additionally, childhood trauma, substance abuse, and urban upbringing have been linked to higher rates of schizophrenia.
Neurobiological abnormalities in the brain are central to the pathophysiology of schizophrenia. Dysregulation of neurotransmitters, particularly dopamine, glutamate, and serotonin, disrupts neural circuits involved in perception, emotion regulation, and cognitive function. Structural brain abnormalities, including enlarged ventricles and decreased gray matter volume, are commonly observed in individuals with schizophrenia.
The interaction between these genetic, environmental, and neurobiological factors contributes to the heterogeneity of schizophrenia presentations and the variability in treatment response among affected individuals. Understanding these diverse influences is crucial for developing targeted interventions and personalized treatment approaches for individuals living with schizophrenia. (Nursing Paper Example on Understanding Schizophrenia: A Comprehensive Overview)
Signs and Symptoms
Schizophrenia presents a diverse array of signs and symptoms that profoundly impact individuals’ lives. Positive symptoms, characterized by an excess or distortion of normal functions, include hallucinations, delusions, disorganized thinking, and speech. Hallucinations can involve hearing voices or seeing things that are not present, while delusions often manifest as fixed false beliefs.
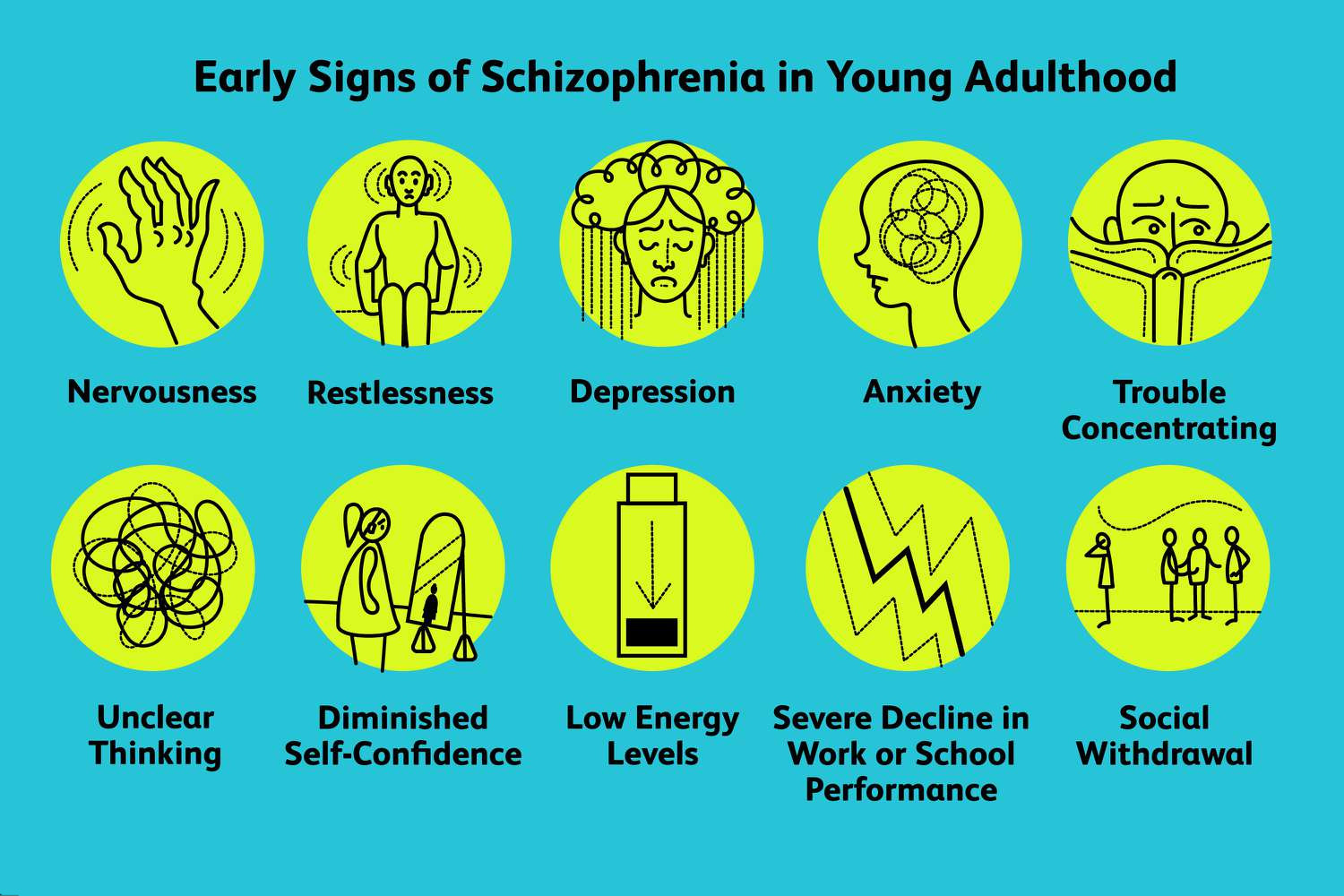
Negative symptoms, marked by a diminishment or absence of normal functions, include flattened affect, social withdrawal, anhedonia (loss of interest or pleasure), and avolition (lack of motivation or goal-directed behavior). These symptoms contribute to a profound impairment in social and occupational functioning, often leading to a loss of autonomy and independence.
Cognitive symptoms are also prominent in schizophrenia and can significantly impact daily functioning. These include deficits in attention, memory, executive function, and processing speed. Individuals may struggle with maintaining focus, remembering information, and making decisions, further hindering their ability to engage in meaningful activities.
Furthermore, mood symptoms frequently accompany schizophrenia, with individuals experiencing symptoms of depression, anxiety, or both. These mood disturbances can exacerbate the severity of the disorder and complicate its management.
The presentation of symptoms can vary widely among individuals with schizophrenia, leading to different clinical subtypes and treatment responses. Some individuals may experience predominantly positive symptoms, while others may exhibit a combination of positive, negative, and cognitive symptoms. The variability in symptomatology underscores the importance of individualized treatment approaches that address the specific needs and challenges of each person living with schizophrenia. Early recognition and intervention are critical for improving outcomes and enhancing quality of life for individuals affected by this complex disorder. (Nursing Paper Example on Understanding Schizophrenia: A Comprehensive Overview)
Etiology
The etiology of schizophrenia is multifactorial, involving a complex interplay of genetic, environmental, and neurobiological factors. Genetic predisposition plays a significant role in the development of schizophrenia, with studies indicating a higher concordance rate among monozygotic twins compared to dizygotic twins. Specific genes related to neurotransmitter systems, such as dopamine, glutamate, and serotonin, as well as genes involved in neurodevelopment and synaptic function, have been implicated in schizophrenia susceptibility.
Environmental factors also contribute to the etiology of schizophrenia. Prenatal exposure to infections, maternal stress during pregnancy, and complications during birth have been associated with an increased risk of developing schizophrenia later in life. Childhood trauma, including physical, emotional, or sexual abuse, has also been linked to the onset of schizophrenia in some individuals. Additionally, substance abuse, particularly cannabis use during adolescence, has been identified as a risk factor for developing schizophrenia.
Neurobiological abnormalities in the brain are central to the pathophysiology of schizophrenia. Dysregulation of neurotransmitter systems, particularly dopamine, glutamate, and serotonin, disrupts neural circuits involved in perception, cognition, and emotion regulation. Structural brain abnormalities, including enlarged ventricles, reduced gray matter volume, and altered connectivity patterns, are commonly observed in individuals with schizophrenia.
The interaction between genetic susceptibility, environmental factors, and neurobiological abnormalities contributes to the heterogeneity of schizophrenia presentations and the variability in treatment response among affected individuals. Understanding the complex etiology of schizophrenia is crucial for developing targeted interventions and personalized treatment approaches that address the specific needs and challenges of individuals living with this disorder. (Nursing Paper Example on Understanding Schizophrenia: A Comprehensive Overview)
Pathophysiology
The pathophysiology of schizophrenia is complex and involves dysregulation across multiple neurobiological systems. Dopamine dysregulation hypothesis suggests that abnormalities in dopamine neurotransmission, particularly in the mesolimbic and mesocortical pathways, contribute to the positive symptoms of schizophrenia. Excessive dopamine activity in the mesolimbic pathway is associated with hallucinations and delusions, while hypoactivity in the mesocortical pathway leads to cognitive deficits and negative symptoms.
Glutamatergic dysfunction is also implicated in schizophrenia pathophysiology. Reduced glutamate levels in certain brain regions, particularly the prefrontal cortex, are associated with cognitive impairments observed in schizophrenia. Glutamate receptors, such as N-methyl-D-aspartate (NMDA) receptors, play a crucial role in synaptic plasticity and cognitive function and are implicated in the pathophysiology of schizophrenia.
Neurodevelopmental abnormalities contribute to the structural and functional alterations observed in the brains of individuals with schizophrenia. Disruptions in early brain development, such as abnormal neuronal migration, synaptic pruning, and myelination, can lead to alterations in brain structure and connectivity. These abnormalities may manifest as enlarged ventricles, reduced gray matter volume, and altered white matter integrity observed in neuroimaging studies of individuals with schizophrenia.
Furthermore, alterations in other neurotransmitter systems, such as serotonin and gamma-aminobutyric acid (GABA), contribute to the complex pathophysiology of schizophrenia. Serotonin dysregulation is implicated in mood disturbances often observed in schizophrenia, while GABAergic dysfunction may contribute to cognitive deficits and affective symptoms.
The intricate interplay of these neurobiological abnormalities underscores the complexity of schizophrenia pathophysiology and highlights the need for comprehensive treatment approaches targeting multiple neurotransmitter systems to address the diverse symptoms of the disorder. (Nursing Paper Example on Understanding Schizophrenia: A Comprehensive Overview)
DSM-5 Diagnosis
The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), provides criteria for the diagnosis of schizophrenia. To meet the criteria for schizophrenia diagnosis, an individual must exhibit characteristic symptoms for a significant portion of time during a one-month period. These symptoms must include at least two of the following: delusions, hallucinations, disorganized speech, grossly disorganized or catatonic behavior, or negative symptoms.
Additionally, the individual must experience significant social or occupational dysfunction due to the symptoms, continuous signs of the disturbance must persist for at least six months, including at least one month of active-phase symptoms (or less if successfully treated), and schizoaffective disorder and depressive or bipolar disorder with psychotic features must be ruled out.
Subtypes of schizophrenia, as outlined in the DSM-5, include paranoid, disorganized, catatonic, undifferentiated, and residual types. Each subtype is characterized by specific symptom patterns and clinical presentations.
Furthermore, the DSM-5 emphasizes the importance of considering the presence of comorbid conditions and differential diagnoses in the assessment of schizophrenia. Other psychiatric disorders with similar symptomatology, such as schizoaffective disorder, bipolar disorder with psychotic features, and substance-induced psychotic disorder, should be ruled out through a comprehensive evaluation.
Accurate diagnosis according to DSM-5 criteria is essential for guiding treatment decisions and interventions tailored to the specific needs of individuals with schizophrenia. A thorough assessment, including a detailed clinical history, psychiatric evaluation, and standardized diagnostic criteria, is crucial for identifying and managing schizophrenia effectively. (Nursing Paper Example on Understanding Schizophrenia: A Comprehensive Overview)
Treatment Regimens and Patient Education
Treatment regimens for schizophrenia typically involve a combination of antipsychotic medications, psychosocial interventions, and support services. Medication adherence and regular therapy sessions are essential for managing symptoms and promoting recovery.
Patient Education
Treatment for schizophrenia typically involves a multimodal approach that combines pharmacotherapy, psychosocial interventions, and patient education to manage symptoms, improve functioning, and promote recovery.
Pharmacotherapy: Antipsychotic medications are the cornerstone of pharmacological treatment for schizophrenia. These medications help alleviate positive symptoms such as hallucinations and delusions by blocking dopamine receptors in the brain. First-generation (typical) and second-generation (atypical) antipsychotics are available, with second-generation agents often preferred due to their lower risk of extrapyramidal side effects. It is essential for individuals with schizophrenia to adhere to their prescribed medication regimen to achieve symptom control and prevent relapse.
Psychosocial Interventions: Psychosocial interventions play a crucial role in schizophrenia management by addressing functional deficits, promoting social integration, and enhancing coping skills. Cognitive-behavioral therapy (CBT), family therapy, and supportive therapy are commonly used approaches to help individuals manage symptoms, improve communication, and enhance problem-solving skills. Social skills training and vocational rehabilitation programs are also beneficial in assisting individuals with schizophrenia in achieving greater independence and community integration.
Patient Education: Patient education is a vital component of schizophrenia management, empowering individuals and their families to understand the nature of the disorder, treatment options, and strategies for coping with symptoms. Education about the importance of medication adherence, potential side effects, and strategies for managing medication-related challenges is essential. Additionally, providing information about the course of the illness, common triggers for relapse, and early warning signs of symptom exacerbation helps individuals and their families recognize when additional support or intervention may be necessary.
Furthermore, educating individuals with schizophrenia about lifestyle factors that can impact their mental health, such as regular exercise, healthy eating habits, adequate sleep, and stress management techniques, promotes overall well-being and symptom stability. Encouraging engagement in social activities, hobbies, and support groups also fosters a sense of belonging and reduces feelings of isolation.
A comprehensive treatment approach for schizophrenia incorporates pharmacotherapy, psychosocial interventions, and patient education to address the multifaceted nature of the disorder and promote optimal outcomes for individuals living with schizophrenia and their families. By combining these treatment modalities, individuals with schizophrenia can achieve symptom control, improve functioning, and enhance their quality of life. (Nursing Paper Example on Understanding Schizophrenia: A Comprehensive Overview)




