Solved Nursing Essay Example on Multiple Sclerosis: Understanding Neurological Disorders
Solved Nursing Essay Example on Multiple Sclerosis: Understanding Neurological Disorders
Multiple sclerosis (MS) is a chronic neurological disorder affecting millions worldwide, characterized by the immune system’s misguided attacks on the central nervous system’s myelin sheath. This autoimmune assault disrupts the transmission of nerve impulses, resulting in a spectrum of debilitating symptoms. Despite extensive research, the precise etiology of MS remains elusive, with genetic predisposition, environmental factors, and immune dysfunction implicated in its onset. The hallmark of MS is its heterogeneity, manifesting in diverse symptoms such as fatigue, sensory disturbances, and motor impairments, making diagnosis and management challenging. As a result, understanding the underlying pathophysiology of MS is critical in developing effective treatment strategies aimed at alleviating symptoms, slowing disease progression, and improving patients’ quality of life. This essay explores the multifaceted aspects of MS, from its causes and symptoms to its diagnosis, treatment regimens, and the importance of patient education in navigating this complex neurological condition. (Solved Nursing Essay Example on Multiple Sclerosis: Understanding Neurological Disorders)
Causes
The causes of multiple sclerosis (MS) are multifactorial and not fully understood, encompassing a complex interplay of genetic, environmental, and immunological factors. While the precise trigger remains elusive, researchers have identified several contributing elements that may predispose individuals to develop MS.
Genetic Predisposition: Genetics play a significant role in MS susceptibility, with studies indicating a higher risk among individuals with a family history of the disease. Specific genetic variations, particularly within the human leukocyte antigen (HLA) complex on chromosome 6, have been linked to an increased susceptibility to MS. However, genetics alone cannot account for the development of MS, suggesting that environmental factors also contribute to its pathogenesis.
Environmental Triggers: Environmental factors are believed to play a crucial role in initiating or exacerbating MS in genetically susceptible individuals. Various environmental triggers have been proposed, including viral infections, particularly Epstein-Barr virus (EBV), which has been consistently associated with an increased risk of MS. Additionally, factors such as low vitamin D levels, smoking, and certain dietary habits have been implicated as potential triggers or modifiers of MS risk.
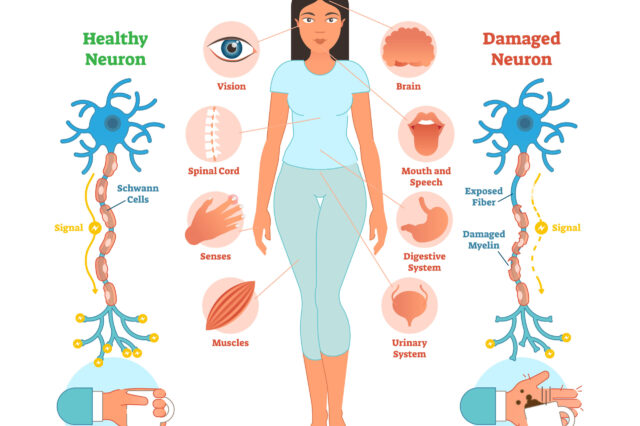
Immunological Dysfunction: MS is fundamentally an autoimmune disorder characterized by aberrant immune responses targeting components of the central nervous system (CNS). In MS, the immune system mistakenly recognizes myelin, the protective sheath surrounding nerve fibers in the CNS, as foreign and launches an attack. This immune-mediated inflammation leads to demyelination, a hallmark feature of MS pathology. Dysregulation of various immune cells, including T cells, B cells, and macrophages, contributes to the chronic inflammation and tissue damage observed in MS.
Complex Interactions: The development of MS likely involves complex interactions between genetic susceptibility and environmental triggers, modulated by immune dysregulation. The exact sequence of events leading to MS onset remains unclear, but it is believed to involve a cascade of inflammatory processes triggered by environmental factors in genetically susceptible individuals.
While the precise etiology of MS remains incompletely understood, it is evident that a combination of genetic predisposition, environmental triggers, and immunological dysfunction contributes to its pathogenesis. Further research is needed to elucidate the intricate mechanisms underlying MS development and identify potential targets for intervention and prevention strategies. (Solved Nursing Essay Example on Multiple Sclerosis: Understanding Neurological Disorders)
Signs and Symptoms
Multiple sclerosis (MS) is characterized by a wide range of signs and symptoms that can vary in severity and presentation, often fluctuating over time. These symptoms result from the immune system’s attack on the central nervous system, leading to disruption in nerve signaling. Understanding the diverse array of symptoms associated with MS is crucial for early diagnosis and effective management of the condition.
Fatigue: Fatigue is one of the most common and debilitating symptoms of MS, affecting up to 80% of individuals with the condition. It is often described as an overwhelming sense of exhaustion that is not relieved by rest and can significantly impact daily activities.
Sensory Disturbances: MS can cause various sensory abnormalities, including numbness, tingling, burning sensations, and altered sensitivity to touch or temperature. These sensations may occur in different parts of the body and can be intermittent or persistent.
Motor Impairments: Motor symptoms in MS may include weakness, muscle stiffness or spasticity, tremors, and difficulty with coordination and balance. These impairments can affect mobility and fine motor skills, leading to challenges in walking, grasping objects, and performing tasks requiring precise movements.
Visual Changes: MS frequently affects vision, leading to symptoms such as blurred or double vision, eye pain, and difficulty with depth perception. Optic neuritis, inflammation of the optic nerve, is a common manifestation of MS and can cause temporary or permanent vision loss.
Cognitive Dysfunction: MS can impact cognitive function, including memory, attention, processing speed, and problem-solving abilities. Cognitive impairment may range from mild difficulties with concentration and multitasking to more severe deficits in memory and executive functioning.
Emotional and Psychological Symptoms: MS can also affect mood and emotional well-being, leading to symptoms such as depression, anxiety, irritability, and mood swings. These psychological symptoms may result from the impact of MS on brain structures involved in regulating emotions.
Other Symptoms: Other common symptoms of MS may include bladder and bowel dysfunction, sexual dysfunction, speech difficulties, and pain, which can manifest as neuropathic pain or musculoskeletal pain.
In summary, the signs and symptoms of MS are diverse and can affect various aspects of an individual’s physical, sensory, cognitive, and emotional functioning. Recognizing and addressing these symptoms early is essential for optimizing treatment outcomes and improving the quality of life for individuals living with MS. (Solved Nursing Essay Example on Multiple Sclerosis: Understanding Neurological Disorders)
Etiology
The etiology of multiple sclerosis (MS) remains complex and multifaceted, involving a combination of genetic predisposition, environmental factors, and immunological dysregulation. Understanding the interplay between these factors is crucial in unraveling the underlying mechanisms driving MS pathogenesis.
Genetic Factors: Genetic susceptibility plays a significant role in MS development, as evidenced by familial clustering and genetic association studies. Certain genetic variations within the human leukocyte antigen (HLA) complex on chromosome 6, particularly the HLA-DRB1*15:01 allele, have been consistently associated with an increased risk of MS. Additionally, genome-wide association studies have identified several other genetic variants linked to MS susceptibility, albeit with modest effect sizes. However, genetics alone cannot account for the entirety of MS risk, indicating the involvement of environmental factors.
Environmental Triggers: Environmental factors are believed to play a pivotal role in initiating or exacerbating MS in genetically susceptible individuals. Among the various environmental triggers implicated in MS pathogenesis, viral infections, particularly Epstein-Barr virus (EBV), have garnered significant attention. EBV infection is more common in individuals with MS compared to the general population, and it is thought to contribute to MS development through mechanisms involving molecular mimicry, immune activation, and dysregulation. Other environmental factors such as low vitamin D levels, smoking, and geographical location (latitude) have also been linked to MS risk, further highlighting the environmental component of MS etiology.
Immunological Dysregulation: MS is fundamentally an autoimmune disorder characterized by aberrant immune responses targeting components of the central nervous system (CNS). Dysregulation of various immune cells, including T cells, B cells, and macrophages, contributes to the chronic inflammation and tissue damage observed in MS. In particular, autoreactive T cells are thought to play a central role in initiating the immune-mediated attack on myelin, leading to demyelination and neurodegeneration. Furthermore, dysregulation of cytokines, chemokines, and other immune mediators further amplifies the inflammatory cascade in MS.
The etiology of MS involves a complex interplay between genetic predisposition, environmental triggers, and immunological dysregulation. Elucidating the intricate mechanisms underlying these factors is essential for advancing our understanding of MS pathogenesis and developing targeted therapeutic strategies. (Solved Nursing Essay Example on Multiple Sclerosis: Understanding Neurological Disorders)
Pathophysiology
The pathophysiology of multiple sclerosis (MS) is characterized by a cascade of events involving immune-mediated inflammation, demyelination, and neurodegeneration within the central nervous system (CNS). Understanding the underlying mechanisms driving these pathological processes is essential for elucidating the disease progression and guiding therapeutic interventions.
Immune-Mediated Inflammation: MS is fundamentally an autoimmune disorder, wherein the immune system mistakenly identifies components of the CNS, particularly myelin, as foreign invaders and launches an inflammatory response. Autoreactive T cells, which normally play a crucial role in defending against pathogens, infiltrate the CNS and initiate an immune attack on myelin-producing oligodendrocytes. This immune-mediated inflammation is characterized by the release of pro-inflammatory cytokines, chemokines, and other immune mediators, leading to tissue damage and activation of resident immune cells within the CNS.
Demyelination: The hallmark pathological feature of MS is demyelination, whereby the myelin sheath surrounding axons in the CNS is damaged or destroyed. Demyelination disrupts the transmission of nerve impulses along axons, leading to impaired neuronal signaling and functional deficits. In addition to oligodendrocyte injury caused by the immune attack, demyelination may also result from secondary processes such as oxidative stress, excitotoxicity, and mitochondrial dysfunction.
Neurodegeneration: In addition to demyelination, MS is associated with neurodegenerative processes involving axonal injury and neuronal loss. Axonal damage can occur as a direct consequence of demyelination, leading to axonal transection, conduction block, and eventual axonal degeneration. Neurodegeneration is thought to contribute to the progressive accumulation of disability in MS patients, independent of the inflammatory demyelinating process. Chronic inflammation, excitotoxicity, and mitochondrial dysfunction are among the mechanisms implicated in neurodegeneration in MS.
Gliosis and Scar Formation: In response to the immune-mediated injury and demyelination, reactive gliosis occurs, characterized by the proliferation and activation of astrocytes and microglia. This glial response contributes to the formation of gliotic scars, which further disrupt normal neuronal function and impede remyelination processes in MS.
The pathophysiology of MS involves a complex interplay of immune-mediated inflammation, demyelination, neurodegeneration, and gliotic scar formation within the CNS. Elucidating the underlying mechanisms driving these pathological processes is crucial for developing targeted therapeutic strategies aimed at modulating disease progression and preserving neurological function in MS patients. (Solved Nursing Essay Example on Multiple Sclerosis: Understanding Neurological Disorders)
DSM-5 Diagnosis
The diagnosis of multiple sclerosis (MS) is based on clinical evaluation, neurological examination, and diagnostic criteria established by the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5). DSM-5 criteria provide a standardized framework for identifying and classifying MS based on the characteristic clinical features and neuroimaging findings associated with the disease.
Clinical Presentation: The DSM-5 outlines specific criteria for diagnosing MS, which include the presence of symptoms attributable to lesions within the central nervous system (CNS) and evidence of dissemination of these lesions in both space and time. Common clinical manifestations of MS include sensory disturbances, motor impairments, visual changes, fatigue, and cognitive dysfunction. The onset of symptoms may be acute or insidious, with exacerbations and remissions being characteristic of the disease course.
Neurological Examination: A comprehensive neurological examination is essential in the diagnosis of MS, as it helps assess the presence and severity of neurological deficits indicative of CNS involvement. Neurological signs commonly observed in MS patients include abnormalities in gait, coordination, muscle strength, reflexes, and sensation. Additionally, specific clinical signs such as optic neuritis, internuclear ophthalmoplegia, and Lhermitte’s sign may be indicative of MS pathology.
Diagnostic Testing: In addition to clinical evaluation, diagnostic testing plays a crucial role in confirming the diagnosis of MS. Magnetic resonance imaging (MRI) of the brain and spinal cord is the primary imaging modality used to detect characteristic MS lesions, including T2 hyperintense lesions, gadolinium-enhancing lesions indicative of active inflammation, and T1 hypointense lesions suggestive of chronic demyelination. Cerebrospinal fluid (CSF) analysis may also be performed to assess for the presence of oligoclonal bands and elevated levels of IgG, indicative of an inflammatory process within the CNS.
Criteria for MS Diagnosis: According to DSM-5 criteria, a diagnosis of MS requires the presence of specific clinical symptoms and evidence of CNS lesions disseminated in both space and time, as demonstrated by clinical evaluation, neurological examination, and diagnostic imaging. Meeting these criteria is essential for establishing a definitive diagnosis of MS and guiding appropriate management and treatment strategies for affected individuals. (Solved Nursing Essay Example on Multiple Sclerosis: Understanding Neurological Disorders)
Treatment Regimens
Management of multiple sclerosis (MS) aims to alleviate symptoms, modify disease progression, and improve patients’ quality of life through a combination of pharmacological and non-pharmacological interventions.
Pharmacological Interventions:
- Disease-Modifying Therapies (DMTs): DMTs are a cornerstone of MS treatment, aimed at reducing disease activity, relapse rates, and disability progression. These medications, including interferons, glatiramer acetate, dimethyl fumarate, fingolimod, and others, target the immune system to modulate inflammation and prevent further damage to the central nervous system (CNS).
- Symptomatic Management: Symptomatic treatments are prescribed to alleviate specific MS symptoms, such as fatigue, spasticity, neuropathic pain, bladder dysfunction, and depression. Medications, physical therapy, occupational therapy, and assistive devices may be utilized to address these symptoms and improve patients’ functional abilities and overall well-being.
- Acute Relapse Management: In the event of an acute relapse or exacerbation of MS symptoms, high-dose corticosteroids, such as intravenous methylprednisolone, are often prescribed to reduce inflammation and hasten recovery. Plasma exchange (plasmapheresis) may be considered in refractory cases or when corticosteroids are contraindicated.
Non-Pharmacological Interventions:
- Rehabilitation Therapies: Physical therapy, occupational therapy, and speech therapy play a vital role in managing MS-related impairments and disabilities. These therapies focus on improving mobility, strength, coordination, fine motor skills, and communication abilities, thereby enhancing patients’ independence and quality of life.
- Exercise and Lifestyle Modifications: Regular exercise, tailored to individual abilities and preferences, has been shown to improve MS symptoms, physical function, and overall well-being. Additionally, adopting a healthy lifestyle, including a balanced diet, adequate hydration, stress management, and smoking cessation, can help optimize health outcomes in MS patients.
- Supportive Care: Psychosocial support, counseling, and support groups can provide valuable emotional and social support to MS patients and their caregivers. Addressing mental health issues, coping strategies, and social isolation can significantly improve patients’ mental and emotional well-being. (Solved Nursing Essay Example on Multiple Sclerosis: Understanding Neurological Disorders)
:max_bytes(150000):strip_icc()/rehabilitation-therapies-for-multiple-sclerosis-4072854-e72137c8397a4d909ce759135c9fa3a8.png)
Patient Education
Patient education is essential in empowering individuals with MS to actively participate in their treatment and self-management. Key components of patient education include:
- Understanding MS: Providing comprehensive information about the nature of MS, its causes, symptoms, disease course, and potential complications helps patients and their families better understand the condition and its impact on daily life.
- Treatment Options: Educating patients about available treatment options, including DMTs, symptomatic therapies, and non-pharmacological interventions, enables informed decision-making and encourages adherence to treatment regimens.
- Self-Management Strategies: Teaching patients self-management techniques, such as medication adherence, symptom monitoring, stress management, and lifestyle modifications, empowers them to take an active role in managing their condition and optimizing health outcomes.
- Symptom Recognition and Management: Educating patients about common MS symptoms, their triggers, and effective management strategies help patients recognize early warning signs of disease exacerbations and take appropriate actions to mitigate symptoms.
- Disease Monitoring: Regular monitoring of disease activity, through clinical assessments, neurological examinations, imaging studies, and laboratory tests, helps patients and healthcare providers track disease progression, evaluate treatment efficacy, and make informed adjustments to treatment plans as needed.
A comprehensive approach to MS management involves a combination of pharmacological and non-pharmacological interventions, along with patient education aimed at promoting self-management, optimizing treatment outcomes, and improving patients’ quality of life. By providing patients with the knowledge, skills, and support needed to actively participate in their care, healthcare providers can help individuals with MS navigate the complexities of their condition and achieve better health outcomes. (Solved Nursing Essay Example on Multiple Sclerosis: Understanding Neurological Disorders)
Conclusion
Multiple sclerosis (MS) presents a complex challenge in neurological healthcare, affecting millions worldwide. This essay has explored various aspects of MS, including its causes, signs and symptoms, etiology, pathophysiology, DSM-5 diagnosis, treatment regimens, and patient education. Understanding the interplay between genetic predisposition, environmental triggers, and immunological dysregulation is crucial in unraveling the underlying mechanisms driving MS pathogenesis. Additionally, effective management of MS involves a combination of pharmacological interventions, rehabilitation therapies, and lifestyle modifications aimed at alleviating symptoms, modifying disease progression, and improving patients’ quality of life. Moreover, patient education plays a pivotal role in empowering individuals with MS to actively participate in their care and make informed decisions regarding treatment options and self-management strategies. Overall, addressing the complex needs of MS patients requires a holistic approach that integrates medical expertise, patient education, and supportive care to optimize health outcomes and enhance overall well-being. (Solved Nursing Essay Example on Multiple Sclerosis: Understanding Neurological Disorders)
References
https://www.ncbi.nlm.nih.gov/books/NBK499849/




