Nursing Paper Example on Atherosclerosis: Unveiling the Silent Threat
Nursing Paper Example on Atherosclerosis: Unveiling the Silent Threat
Causes
Signs and Symptoms
Atherosclerosis, often insidious in its onset, manifests through a spectrum of clinical signs and symptoms reflecting compromised blood flow to vital organs. Initially asymptomatic, the disease stealthily progresses until it culminates in life-threatening events. Common indicators of atherosclerosis include angina, intermittent claudication, and critical organ ischemia.
Angina, characterized by chest discomfort or pressure, arises from myocardial ischemia secondary to coronary artery atherosclerosis. Typically triggered by physical exertion or emotional stress, angina presents as a tightness or squeezing sensation in the chest, often radiating to the arms, neck, jaw, or back. Despite being transient, angina warrants prompt medical evaluation to assess underlying coronary artery disease severity and risk of acute coronary events.
Intermittent claudication, a hallmark of peripheral artery disease, manifests as muscle pain or cramping during physical activity, particularly in the lower extremities. Diminished blood flow to leg muscles results in inadequate oxygen delivery, precipitating discomfort that subsides with rest. Intermittent claudication imposes limitations on mobility and physical function, significantly impairing quality of life.
Critical organ ischemia represents advanced atherosclerosis complications, posing imminent threats to organ viability. Myocardial infarction, a catastrophic consequence of coronary artery atherosclerosis, occurs when plaque rupture triggers thrombotic occlusion of a coronary artery, leading to myocardial tissue necrosis. Ischemic stroke, stemming from cerebral artery atherosclerosis or embolic phenomena, manifests with focal neurological deficits such as hemiparesis, aphasia, or visual disturbances. Similarly, acute limb ischemia, precipitated by peripheral artery occlusion, presents with acute limb pain, pallor, pulselessness, and paralysis, necessitating emergent revascularization interventions to salvage limb function.
In summary, atherosclerosis presents with diverse clinical manifestations ranging from exertional chest pain and intermittent claudication to life-threatening events like myocardial infarction, stroke, and acute limb ischemia. Recognizing these signs and symptoms is crucial for timely diagnosis and intervention, mitigating the morbidity and mortality associated with advanced atherosclerosis complications. (Nursing Paper Example on Atherosclerosis: Unveiling the Silent Threat)
Etiology
The etiology of atherosclerosis is multifactorial, encompassing intricate interactions between genetic predispositions, environmental factors, and systemic processes. Genetic influences exert a significant impact on atherosclerosis susceptibility and progression, with variations in genes encoding lipid metabolism enzymes, inflammatory mediators, and endothelial function regulators contributing to disease pathogenesis. Familial hypercholesterolemia, an inherited disorder characterized by elevated LDL cholesterol levels, exemplifies the genetic underpinnings of atherosclerosis, underscoring the role of genetic predispositions in lipid metabolism abnormalities.
Environmental factors play a pivotal role in shaping atherosclerosis risk profiles, with lifestyle choices exerting profound influences on disease development and progression. Tobacco smoke, laden with toxic compounds, accelerates atherosclerosis through endothelial dysfunction, oxidative stress, and enhanced inflammatory responses. High-fat diets rich in saturated fats and trans fats exacerbate dyslipidemia, fostering lipid deposition within arterial walls and promoting plaque formation. Sedentary lifestyles and physical inactivity contribute to metabolic derangements, insulin resistance, and systemic inflammation, amplifying atherosclerosis risk.
Systemic processes, including chronic inflammation and oxidative stress, fuel atherosclerosis progression by perpetuating endothelial dysfunction and promoting plaque instability. Inflammatory mediators, such as C-reactive protein and interleukins, orchestrate inflammatory responses within arterial walls, attracting circulating immune cells and promoting foam cell formation. Oxidative stress, induced by reactive oxygen species, oxidizes circulating lipids, rendering them more atherogenic and facilitating their incorporation into developing plaques.
Furthermore, metabolic disorders such as diabetes mellitus and hypertension exacerbate atherosclerosis by amplifying endothelial dysfunction, oxidative stress, and inflammatory responses. Hyperglycemia, a hallmark of diabetes mellitus, promotes endothelial injury and accelerates atherosclerosis progression through glycation of vascular proteins and activation of proinflammatory pathways. Hypertension, characterized by elevated blood pressure, subjects arterial walls to chronic hemodynamic stress, fostering endothelial dysfunction and facilitating lipid infiltration.
In summary, the etiology of atherosclerosis encompasses a complex interplay of genetic predispositions, environmental influences, and systemic processes, highlighting the multifactorial nature of this pervasive cardiovascular disease. Understanding these etiological factors is paramount in devising targeted preventive and therapeutic interventions to mitigate atherosclerosis-related morbidity and mortality. (Nursing Paper Example on Atherosclerosis: Unveiling the Silent Threat)
Pathophysiology
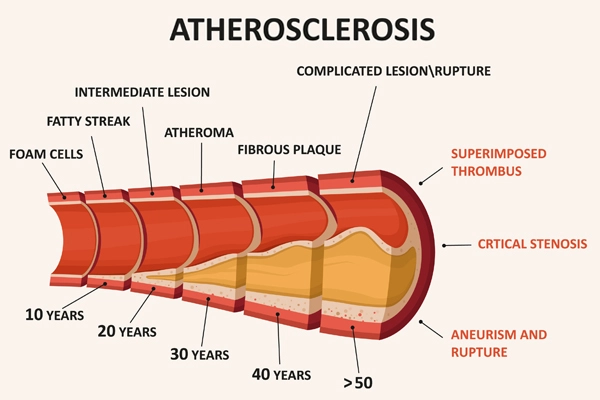
Atherosclerosis unfolds through a multifaceted pathophysiological cascade characterized by endothelial dysfunction, lipid accumulation, inflammatory responses, and plaque formation within arterial walls. Endothelial dysfunction, triggered by various insults including hemodynamic stressors and metabolic disturbances, represents a critical initiating event in atherosclerosis pathogenesis. Impaired endothelial integrity promotes the adhesion of circulating monocytes and leukocytes to the endothelial surface, initiating an inflammatory response within arterial walls.
After endothelial dysfunction, lipids, particularly low-density lipoprotein (LDL) cholesterol, infiltrate the subendothelial space and undergo oxidative modifications, rendering them more atherogenic. Oxidized LDL cholesterol induces a robust inflammatory response, attracting monocytes to the arterial intima. Monocytes differentiate into macrophages upon entering the subendothelial space, where they engulf oxidized LDL cholesterol and transform into foam cells, hallmark features of early atherosclerotic lesions.
Accumulation of foam cells within the arterial wall triggers a cascade of events leading to plaque formation. Foam cells release proinflammatory cytokines and growth factors, perpetuating local inflammation and promoting smooth muscle cell migration from the media to the intima. Smooth muscle cells proliferate and synthesize extracellular matrix components, contributing to the formation of a fibrous cap overlaying the lipid-rich core of the developing plaque.
As the atherosclerotic lesion progresses, the fibrous cap undergoes remodeling, becoming susceptible to rupture. Plaque rupture exposes the thrombogenic lipid core to the circulating blood, precipitating thrombus formation and occlusion of the affected artery. Thrombotic occlusion results in acute ischemic events such as myocardial infarction, stroke, or acute limb ischemia, underscoring the clinical significance of advanced atherosclerosis complications.
In summary, atherosclerosis pathophysiology involves a complex interplay of endothelial dysfunction, lipid accumulation, inflammatory responses, and plaque formation within arterial walls. Understanding these pathophysiological mechanisms is crucial in elucidating disease progression and devising targeted therapeutic strategies to mitigate atherosclerosis-related morbidity and mortality. (Nursing Paper Example on Atherosclerosis: Unveiling the Silent Threat)
DMS-5 Diagnosis
The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DMS-5), provides a structured framework for diagnosing atherosclerosis-related conditions based on clinical criteria and diagnostic tests. Diagnosis typically involves a comprehensive assessment encompassing medical history, physical examination, and ancillary investigations to evaluate cardiovascular risk factors and assess disease severity.
Clinical evaluation begins with a detailed medical history to identify predisposing factors such as smoking, hypertension, diabetes mellitus, and dyslipidemia, which significantly contribute to atherosclerosis development. Moreover, eliciting symptoms suggestive of atherosclerosis-related complications, including angina, intermittent claudication, and critical organ ischemia, aids in establishing the diagnosis.
Physical examination aims to identify objective signs of atherosclerosis and assess cardiovascular risk. Examination of peripheral pulses, auscultation for bruits over major arteries, and evaluation of lower extremity skin perfusion may reveal signs of peripheral artery disease. Moreover, assessment of blood pressure, heart rate, and signs of heart failure or valvular dysfunction provides valuable insights into cardiovascular health.
Ancillary investigations play a pivotal role in confirming the diagnosis and assessing disease severity. Laboratory tests such as lipid profiles, fasting blood glucose, and glycated hemoglobin levels help evaluate metabolic risk factors and assess disease control in individuals with diabetes mellitus. Additionally, electrocardiography (ECG), echocardiography, stress testing, and imaging modalities such as coronary angiography, computed tomography (CT) angiography, and magnetic resonance imaging (MRI) provide valuable diagnostic information regarding coronary artery disease, myocardial ischemia, and atherosclerotic plaque burden.
Integration of clinical findings and diagnostic test results enables clinicians to establish a definitive diagnosis of atherosclerosis and its related complications according to DMS-5 criteria. Accurate diagnosis facilitates risk stratification, guides therapeutic decision-making, and enhances patient outcomes through timely intervention and management of atherosclerosis-related cardiovascular conditions. (Nursing Paper Example on Atherosclerosis: Unveiling the Silent Threat)
Treatment Regimens and Patient Education
Management of atherosclerosis is multifaceted, emphasizing lifestyle modifications, pharmacotherapy, and invasive interventions aimed at mitigating cardiovascular risk factors, halting disease progression, and preventing complications. Additionally, patient education plays a pivotal role in empowering individuals to actively participate in their care and adopt healthy behaviors conducive to cardiovascular wellness.
Lifestyle Modifications: Central to atherosclerosis management, lifestyle modifications target modifiable risk factors such as smoking, unhealthy dietary habits, physical inactivity, and excessive alcohol consumption. Smoking cessation interventions, including counseling and pharmacotherapy, reduce cardiovascular risk and promote vascular health. Adoption of heart-healthy dietary patterns rich in fruits, vegetables, whole grains, and lean proteins, along with limiting saturated fats, trans fats, and sodium, attenuates dyslipidemia and mitigates atherosclerosis progression. Regular physical activity, encompassing aerobic exercise and strength training, improves cardiovascular fitness, insulin sensitivity, and endothelial function, thereby reducing atherosclerosis risk. Furthermore, moderation of alcohol consumption and weight management strategies promote metabolic health and cardiovascular wellness.
Pharmacotherapy: Pharmacological interventions target underlying metabolic abnormalities, lipid imbalances, and cardiovascular risk factors to mitigate atherosclerosis progression and prevent complications. Statins, cornerstone agents in atherosclerosis management, reduce LDL cholesterol levels and stabilize atherosclerotic plaques, thereby lowering cardiovascular event risk. Additionally, antiplatelet agents such as aspirin or P2Y12 inhibitors reduce thrombotic risk in individuals with atherosclerotic cardiovascular disease. Antihypertensive medications, including angiotensin-converting enzyme inhibitors, angiotensin II receptor blockers, beta-blockers, and calcium channel blockers, optimize blood pressure control and mitigate arterial remodeling, fostering cardiovascular health. Moreover, glucose-lowering agents, such as metformin and sodium-glucose cotransporter-2 inhibitors, mitigate atherosclerosis risk in individuals with diabetes mellitus by improving glycemic control and cardiovascular outcomes.
Invasive Interventions: Invasive interventions, including percutaneous coronary intervention (PCI) and coronary artery bypass grafting (CABG), restore blood flow in critically narrowed arteries, relieve ischemic symptoms, and mitigate cardiovascular event risk in individuals with advanced atherosclerosis. PCI involves catheter-based interventions, including balloon angioplasty and stent placement, to alleviate coronary artery stenosis and restore myocardial perfusion. Conversely, CABG utilizes surgically harvested grafts to bypass obstructed coronary arteries, augmenting myocardial blood supply and improving long-term cardiovascular outcomes.
Patient Education: Patient education is integral to atherosclerosis management, fostering informed decision-making, enhancing treatment adherence, and promoting self-management skills crucial for long-term cardiovascular wellness. Educational initiatives encompass comprehensive discussions about atherosclerosis etiology, risk factors, complications, and treatment goals. Individuals are empowered to recognize warning signs of cardiovascular events, adhere to prescribed medications, monitor and manage cardiovascular risk factors, and adopt heart-healthy lifestyles. Furthermore, patient education initiatives emphasize the importance of regular follow-up visits, compliance with diagnostic tests and preventive screenings, and engagement in cardiac rehabilitation programs to optimize cardiovascular health outcomes.
In summary, the management of atherosclerosis encompasses a multifaceted approach integrating lifestyle modifications, pharmacotherapy, and invasive interventions tailored to individual cardiovascular risk profiles and disease severity. Patient education plays a pivotal role in empowering individuals to actively participate in their care, adopt healthy behaviors, and optimize cardiovascular outcomes, underscoring the significance of collaborative efforts between healthcare providers and patients in combating atherosclerosis and promoting cardiovascular wellness. (Nursing Paper Example on Atherosclerosis: Unveiling the Silent Threat)



