Telehealth and Technology in Health Care
Telehealth and Technology in Health Care
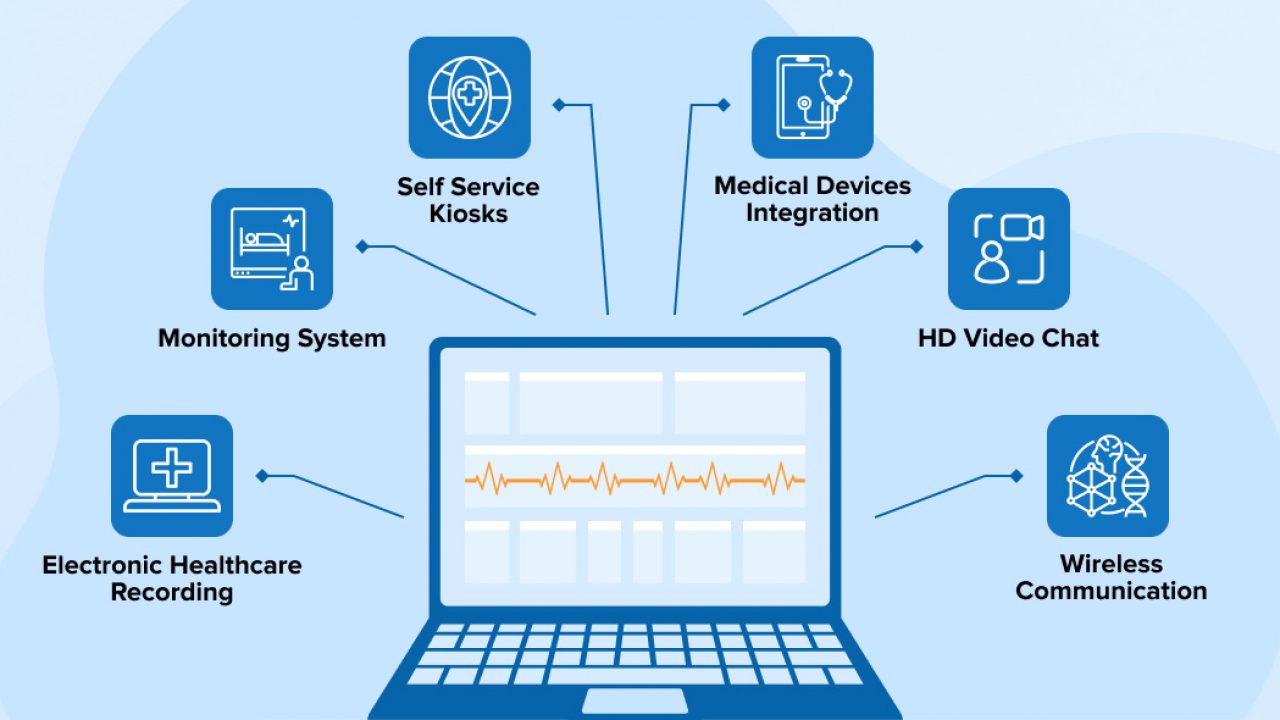
The advent of telehealth and advancements in healthcare technology have ushered in a transformative era in the delivery of medical services. In this digital age, the intersection of healthcare and technology has not only reshaped traditional healthcare practices but has also introduced innovative solutions to enhance patient care and accessibility. Telehealth, encompassing virtual consultations, remote monitoring, and digital health platforms, has emerged as a pivotal tool in bridging geographical gaps and expanding healthcare services to remote or underserved populations. Additionally, cutting-edge technologies such as artificial intelligence, wearable devices, and health informatics are revolutionizing diagnostics, treatment plans, and patient management. This paper explores the profound impact of telehealth and technology on the healthcare landscape, revolutionizing the way medical services are accessed, delivered, and personalized for the benefit of patients and healthcare providers alike.

History and Background
The evolution of telehealth and technology in healthcare is a compelling narrative that spans decades, marked by transformative advancements that have reshaped the delivery of medical services. The roots of telehealth can be traced back to the mid-20th century when the concept of remote patient care began to take shape. The development of telemedicine, an early precursor to telehealth, gained momentum in the 1950s and 1960s with the use of closed-circuit television for consultations between healthcare professionals.
However, it was not until the late 20th century that technological innovations and the widespread adoption of the internet paved the way for the expansion of telehealth services. The advent of the internet allowed for real-time communication and data exchange, enabling healthcare providers to remotely connect with patients and share medical information. The 1990s saw the emergence of telehealth initiatives that focused on delivering healthcare services, consultations, and even surgeries over long distances, particularly to rural or underserved areas.
The early 2000s marked a significant turning point with the proliferation of digital health technologies. The development of electronic health records (EHRs) revolutionized how patient information was stored and shared, streamlining communication among healthcare professionals and improving overall care coordination. Concurrently, the rise of mobile devices and smartphones facilitated the growth of mobile health (mHealth) applications, allowing individuals to monitor their health, track vital signs, and access medical information at their fingertips.
Telehealth continued to evolve with the integration of video conferencing technologies, making virtual consultations more accessible and effective. The widespread adoption of high-speed internet and the refinement of telecommunication infrastructures further fueled the expansion of telehealth services. As a result, remote consultations became commonplace, offering a convenient alternative for routine check-ups, follow-up appointments, and even specialized medical consultations.
The COVID-19 pandemic in the early 21st century acted as a catalyst, accelerating the adoption of telehealth on an unprecedented scale. The need for social distancing and lockdowns prompted healthcare providers to swiftly transition to virtual care, highlighting the flexibility and resilience of telehealth solutions. This period witnessed an exponential increase in the use of telehealth platforms for a wide range of medical services, from primary care to mental health consultations.
In tandem with the telehealth revolution, technology has continued to drive innovation within healthcare. Artificial intelligence (AI) and machine learning are being increasingly employed for predictive analytics, personalized treatment plans, and diagnostic assistance. Wearable devices equipped with sensors and health monitoring capabilities empower individuals to actively participate in their healthcare, providing real-time data to healthcare providers for more informed decision-making.
Generally, the history of telehealth and technology in healthcare reflects a journey of continuous innovation and adaptation. From the early experiments with closed-circuit television to the widespread adoption of virtual care platforms, the landscape has evolved significantly. As technology continues to advance, the future of telehealth holds promise for further breakthroughs, offering new possibilities for personalized, efficient, and accessible healthcare services.
Factors Contributing to the Increased Utilization of Telehealth and Technology in Healthcare
The increased utilization of telehealth and technology in healthcare is a multifaceted phenomenon driven by a convergence of factors that collectively reshape the traditional paradigms of healthcare delivery. A pivotal catalyst for this transformation is the widespread growth of digital connectivity and internet accessibility. The availability of high-speed internet has become ubiquitous, enabling seamless communication and data exchange between healthcare providers and patients. This fundamental infrastructure forms the backbone of telehealth services, facilitating real-time virtual consultations, remote patient monitoring, and the exchange of critical medical information. As a result, geographical barriers are diminished, and healthcare access is extended to remote or underserved populations.
Furthermore, the growing demand for patient-centric and convenient healthcare solutions contributes significantly to the increased utilization of telehealth and technology. In an era where individuals are accustomed to the convenience afforded by digital technologies in various aspects of their lives, there is a corresponding expectation for healthcare services that align with their preferences for flexibility and accessibility. Telehealth platforms provide an avenue for patients to connect with healthcare professionals from the comfort of their homes, eliminating the need for travel and minimizing disruptions to their daily routines. The appeal of on-demand virtual care options has resonated with a broad spectrum of the population, fostering a shift in the perception of healthcare as a service that can be accessed conveniently and promptly.
The unprecedented challenges brought about by the COVID-19 pandemic further accelerated the adoption of telehealth, catapulting it into the forefront of healthcare delivery. The imperative for social distancing and the need to reduce the risk of viral transmission prompted healthcare providers to swiftly embrace virtual care solutions to ensure the continuity of patient care. This forced paradigm shift underscored the adaptability and resilience of telehealth technologies, leading to widespread recognition of their benefits and creating a lasting impact on healthcare delivery models. Patients and providers alike became more receptive to the notion of virtual consultations, and the acceptance of telehealth as a mainstream healthcare modality was solidified.
Technological advancements, particularly in the realms of artificial intelligence (AI) and machine learning, play a crucial role in driving the increased utilization of technology in healthcare. AI applications are increasingly harnessed for predictive analytics, diagnostics, and the development of personalized treatment plans. These technologies enhance the efficiency and effectiveness of healthcare services, supporting healthcare providers in delivering more precise and targeted interventions. Wearable devices equipped with health monitoring capabilities have empowered individuals to actively engage in their healthcare management. These devices provide real-time data on vital signs, activity levels, and other health metrics, offering valuable insights to both patients and healthcare professionals for more informed decision-making.
Moreover, regulatory changes and policy initiatives have acted as important facilitators in fostering the adoption of telehealth. The removal of barriers, the implementation of reimbursement policies for virtual care services, and the provision of regulatory frameworks for telehealth practices have incentivized healthcare providers to integrate telehealth into their practice. These supportive measures ensure financial sustainability and viability for healthcare organizations embracing telehealth, fostering a conducive environment for its widespread adoption.
Conclusively, the increased utilization of telehealth and technology in healthcare is a dynamic and multifaceted phenomenon driven by the convergence of digital connectivity, changing patient expectations, the impact of the COVID-19 pandemic, technological advancements, and supportive regulatory measures. As these factors continue to evolve, the trajectory of healthcare delivery is likely to be shaped by the ongoing integration of innovative technologies. The collaborative efforts of healthcare providers, technology developers, policymakers, and patients will play a pivotal role in harnessing the full potential of telehealth and technology to create a healthcare landscape that is more accessible, efficient, and patient-centered.
Barriers to Telehealth and Technology in Healthcare
Despite the transformative potential of telehealth and technology in healthcare, several barriers impede their widespread adoption and integration into traditional healthcare systems. One significant challenge is the digital divide, where disparities in access to technology and high-speed internet hinder certain populations from benefiting fully. Individuals in rural or economically disadvantaged areas may lack the necessary infrastructure for seamless telehealth interactions, limiting their ability to engage in virtual consultations and access digital health resources.
Interoperability issues among different healthcare systems and electronic health records (EHRs) present a substantial barrier to the seamless exchange of patient information. Incompatibility between various technologies used by healthcare providers can hinder the efficient sharing of critical data, reducing the effectiveness of telehealth interventions and compromising continuity of care.
Furthermore, concerns related to data security and patient privacy act as significant barriers to the widespread adoption of technology in healthcare. Patients and healthcare providers alike worry about the confidentiality and protection of sensitive health information in the digital realm. Ensuring robust cybersecurity measures and compliance with privacy regulations is paramount to building trust in telehealth and technology-enabled healthcare solutions.
Resistance to change within the healthcare industry is another notable barrier. The traditional healthcare system is deeply ingrained in established practices, and the introduction of new technologies requires a cultural shift. Healthcare professionals may face challenges adapting to new workflows, technology interfaces, and remote care models. Adequate training and education are essential to overcoming this barrier and fostering a culture of acceptance and proficiency in leveraging technology.
Reimbursement policies and regulatory frameworks pose significant challenges to the sustainable integration of telehealth into mainstream healthcare. Variability in reimbursement policies across regions, uncertainty about the longevity of temporary pandemic-related reimbursement measures, and the lack of standardized guidelines hinder the financial viability of telehealth practices. Clear and consistent regulatory frameworks are needed to address these concerns and provide a foundation for the stable integration of telehealth into routine healthcare delivery.
Generally, while telehealth and technology offer immense potential to enhance healthcare accessibility and efficiency, various barriers persist. Overcoming issues related to the digital divide, interoperability, data security, resistance to change, and regulatory challenges is crucial for unlocking the full benefits of these innovations. Collaborative efforts between healthcare stakeholders, technology developers, policymakers, and regulatory bodies are essential to address these barriers systematically and ensure that telehealth becomes an integral and sustainable component of modern healthcare delivery.
Telehealth and HIPAA
Telehealth, while offering valuable benefits in terms of accessibility and convenience, introduces complex considerations regarding patient privacy and data security, particularly in relation to the Health Insurance Portability and Accountability Act (HIPAA) in the United States. HIPAA is a federal law that safeguards protected health information (PHI) and ensures the confidentiality and security of patients’ sensitive data.
Telehealth services must adhere to HIPAA regulations to protect patient privacy during virtual consultations. This includes implementing secure communication channels, utilizing encrypted platforms, and ensuring that only authorized individuals have access to patient information. Healthcare providers employing telehealth solutions are required to conduct risk assessments and implement measures to safeguard electronic PHI (ePHI) from unauthorized access or disclosure.
In response to the COVID-19 pandemic, the Department of Health and Human Services (HHS) temporarily relaxed certain HIPAA requirements to facilitate the rapid deployment of telehealth services. However, healthcare providers must remain vigilant in adopting HIPAA-compliant telehealth technologies to maintain the integrity of patient privacy. As the landscape evolves, a balance between innovation and regulatory compliance is crucial to ensure that telehealth continues to provide accessible and secure healthcare services while upholding the principles of patient confidentiality outlined in HIPAA.

Telehealth in Nursing
Telehealth has emerged as a transformative force in nursing, revolutionizing the way healthcare services are delivered and expanding the scope of nursing practice. One of the key advantages of telehealth in nursing is its ability to enhance accessibility to care. Nurses can remotely connect with patients, providing consultations, monitoring chronic conditions, and offering guidance on self-care strategies, thereby overcoming geographical barriers and reaching individuals in remote or underserved areas.
In primary care, telehealth allows nurses to conduct virtual assessments, offer preventive care advice, and follow up with patients for routine check-ups. It improves patient convenience and contributes to more efficient healthcare delivery. Additionally, telehealth enables nurses to engage in proactive health management, fostering patient education and empowering individuals to take an active role in their well-being.
In specialty areas such as mental health nursing, telehealth has proven especially valuable. Psychiatric nurses can conduct virtual therapy sessions, assessments, and medication management, providing timely and accessible mental health support. The confidential and convenient nature of telehealth in mental health nursing encourages more individuals to seek assistance, reducing barriers associated with stigma or travel constraints.
Moreover, telehealth supports collaborative care models by facilitating communication among healthcare team members. Nurses can virtually consult with physicians, share patient data, and coordinate care plans, fostering a holistic and patient-centered approach. This collaborative aspect is particularly beneficial for complex cases, ensuring that interdisciplinary teams can efficiently work together to address diverse healthcare needs.
However, the integration of telehealth in nursing is not without challenges. Nurses need to adapt to new technologies, acquire proficiency in virtual communication, and ensure that the virtual environment maintains the same standards of patient-centered care and empathy as in-person interactions. Regulatory considerations, including compliance with privacy laws such as the Health Insurance Portability and Accountability Act (HIPAA), also play a crucial role in shaping telehealth practices in nursing.
Generally, telehealth has become an integral component of modern nursing practice, offering nurses innovative tools to deliver patient-centered care, enhance accessibility, and contribute to more collaborative and efficient healthcare systems. As technology continues to evolve, nurses will likely play an increasingly prominent role in shaping the future of telehealth, leveraging its potential to improve patient outcomes and address the dynamic healthcare needs of diverse populations.
Conclusion
This assessment reveals a transformative landscape where digital innovations play a pivotal role in reshaping the delivery of medical services. From the historical evolution and barriers to increased utilization in healthcare, it is evident that telehealth and technology hold immense promise for enhancing accessibility, efficiency, and patient-centered care. The integration of artificial intelligence, wearables, and virtual consultations represents a paradigm shift that transcends geographical limitations, addresses disparities, and fosters proactive health management. However, challenges such as the digital divide, interoperability issues, and regulatory considerations must be navigated. As the healthcare industry continues to embrace these advancements, collaborative efforts among healthcare professionals, technology developers, policymakers, and patients are essential to unlock the full potential of telehealth and technology, ensuring a future where healthcare is both innovative and inclusive.
Top of Form


