Nursing Paper Example on Bell’s Palsy: Understanding its Causes, Symptoms, and Management
Nursing Paper Example on Bell’s Palsy: Understanding its Causes, Symptoms, and Management
Causes
The precise cause of Bell’s palsy remains uncertain, but it is widely believed to be related to inflammation and swelling of the facial nerve, known as the seventh cranial nerve. This inflammation disrupts the normal function of the nerve, leading to paralysis or weakness of the facial muscles on one side of the face. While the exact trigger for this inflammation is not fully understood, several factors have been proposed as potential causes or contributing factors to the development of Bell’s palsy.
Viral infections, particularly herpes simplex virus (HSV), are frequently associated with the onset of Bell’s palsy. It is theorized that viral replication within the facial nerve or surrounding tissue triggers an inflammatory response, leading to nerve damage and dysfunction. Other viruses, including herpes zoster virus (which causes shingles), Epstein-Barr virus (associated with infectious mononucleosis), and cytomegalovirus, have also been implicated in some cases.
Additionally, certain conditions and risk factors may predispose individuals to developing Bell’s palsy. These include diabetes mellitus, hypertension, pregnancy, upper respiratory tract infections, autoimmune diseases, and a family history of the condition. While the exact mechanism by which these factors contribute to Bell’s palsy is not fully understood, it is believed that they may exacerbate inflammation or compromise the immune response, increasing susceptibility to nerve damage.
Furthermore, anatomical factors such as the course of the facial nerve as it passes through the temporal bone and its proximity to other structures within the skull may also play a role in the development of Bell’s palsy. Compression or irritation of the facial nerve due to these anatomical features could potentially lead to nerve dysfunction and the characteristic symptoms of Bell’s palsy.
In summary, while viral infections, particularly HSV, are commonly associated with Bell’s palsy, a combination of genetic predisposition, environmental factors, and anatomical considerations may contribute to its onset. Further research is needed to elucidate the exact mechanisms underlying this condition and identify potential preventive strategies. (Nursing Paper Example on Bell’s Palsy: Understanding its Causes, Symptoms, and Management)
Signs and Symptoms
Bell’s palsy presents with distinctive signs and symptoms, typically characterized by sudden onset unilateral facial weakness or paralysis. The onset of symptoms is often rapid, occurring for hours to days, and may progress gradually or reach maximum severity within a short time frame.
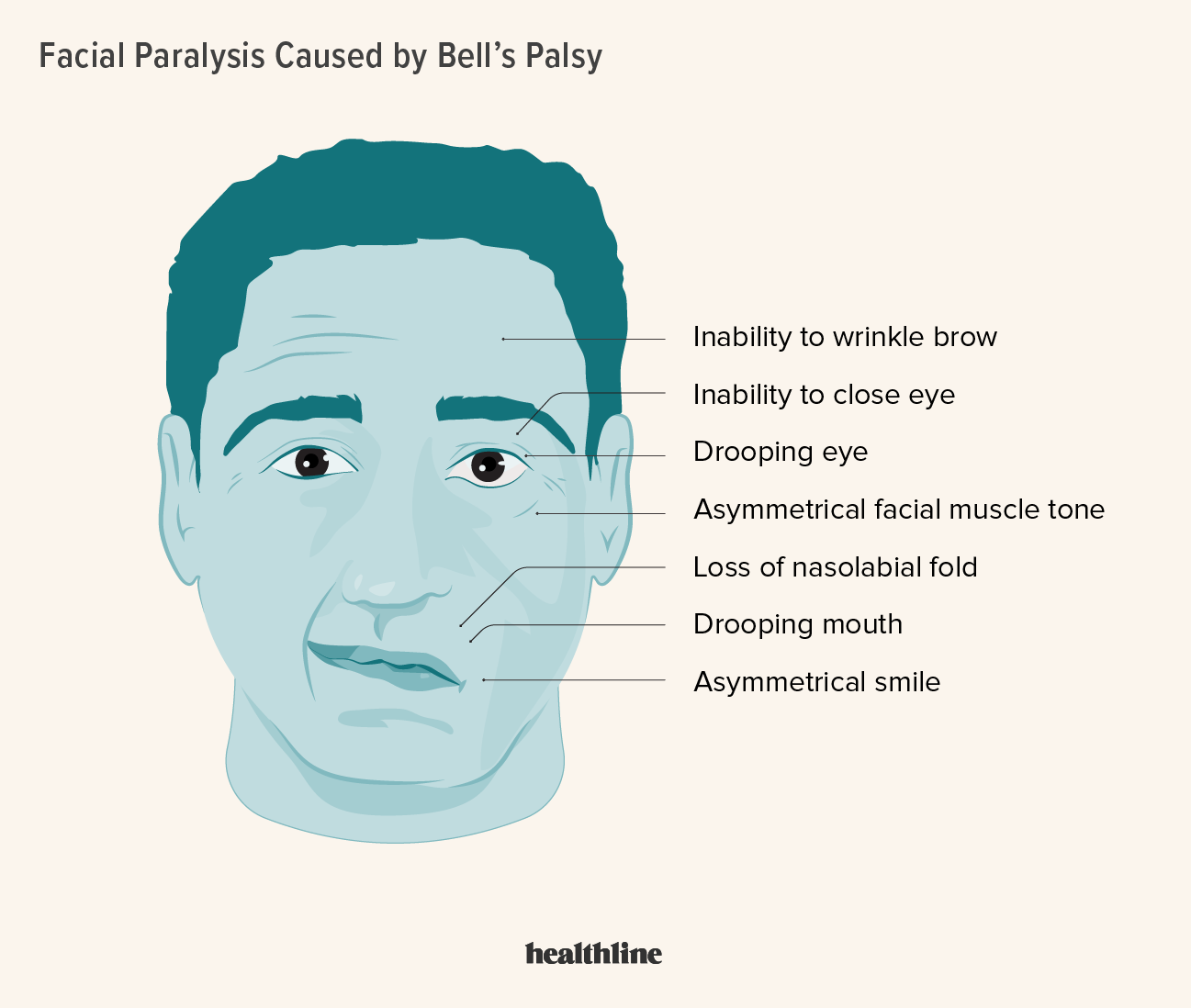
Common manifestations of Bell’s palsy include asymmetry of facial expressions, with one side of the face appearing droopy or slack compared to the other side. This asymmetry can affect various facial movements, including smiling, raising the eyebrows, and closing the eye on the affected side. Patients may also experience difficulty in controlling facial muscles, leading to an inability to fully close one eye or difficulty with tasks such as blowing out candles or whistling.
In addition to facial weakness or paralysis, individuals with Bell’s palsy may report other associated symptoms, including facial pain or discomfort, particularly around the ear or jaw on the affected side. Some patients may also experience altered sensations, such as tingling or numbness, in the facial region.
One of the hallmark signs of Bell’s palsy is the presence of unilateral facial drooping or weakness that worsens with facial movements but improves or resolves during periods of rest. This fluctuating nature of symptoms distinguishes Bell’s palsy from other causes of facial paralysis, such as stroke or traumatic injury, which typically present with more persistent deficits.
Furthermore, Bell’s palsy may be accompanied by other sensory or motor disturbances, such as impaired taste perception on the anterior two-thirds of the tongue or increased sensitivity to sounds (hyperacusis) on the affected side. These additional symptoms can vary in severity and may not be present in all cases of Bell’s palsy. (Nursing Paper Example on Bell’s Palsy: Understanding its Causes, Symptoms, and Management)
Etiology
The etiology of Bell’s palsy is multifactorial and involves a complex interplay of genetic, environmental, and immunological factors. While the exact cause of the condition remains elusive, several hypotheses have been proposed to explain its pathogenesis.
One of the leading theories suggests that Bell’s palsy is triggered by viral infections, particularly herpes simplex virus (HSV). It is believed that viral replication within the facial nerve or surrounding tissue induces an inflammatory response, leading to edema and compression of the nerve. This inflammatory cascade ultimately results in nerve dysfunction and the characteristic facial paralysis observed in Bell’s palsy. Other viruses, including herpes zoster virus (which causes shingles), Epstein-Barr virus, and cytomegalovirus, have also been implicated in some cases.
In addition to viral infections, genetic predisposition may play a role in the development of Bell’s palsy. Studies have identified certain genetic polymorphisms associated with an increased risk of developing the condition, suggesting a hereditary component. However, the specific genes involved and their exact role in Bell’s palsy remain poorly understood.
Environmental factors, such as cold weather, upper respiratory tract infections, and trauma to the face or head, have also been implicated as potential triggers for Bell’s palsy. These factors may exacerbate inflammation or compromise the immune response, increasing susceptibility to nerve damage.
Furthermore, anatomical considerations may contribute to the development of Bell’s palsy. The facial nerve travels through a narrow bony canal within the temporal bone, leaving it susceptible to compression or irritation from surrounding structures. Additionally, the proximity of the facial nerve to other cranial nerves and blood vessels within the skull may increase the risk of nerve injury in certain individuals.
In summary, Bell’s palsy is likely the result of a complex interplay between viral infections, genetic predisposition, environmental factors, and anatomical considerations. Further research is needed to elucidate the specific mechanisms underlying the development of this condition and identify potential targets for therapeutic intervention. (Nursing Paper Example on Bell’s Palsy: Understanding its Causes, Symptoms, and Management)
Pathophysiology
Bell’s palsy is characterized by inflammation and dysfunction of the facial nerve, also known as the seventh cranial nerve, which controls the muscles responsible for facial expressions. The exact pathophysiological mechanisms underlying Bell’s palsy are not fully understood, but several key processes are thought to have contributed to its development.
The initial trigger for Bell’s palsy is believed to be viral infections, particularly herpes simplex virus (HSV), which leads to inflammation of the facial nerve and surrounding tissues. Viral replication within the nerve or adjacent structures triggers an immune response, resulting in the release of pro-inflammatory cytokines and the recruitment of immune cells to the site of infection.
This inflammatory cascade causes edema and swelling of the facial nerve, leading to compression within the narrow confines of the facial canal as it passes through the temporal bone. The compression of the nerve disrupts its normal function, impairing the transmission of signals from the brain to the facial muscles.
As a result, patients with Bell’s palsy experience weakness or paralysis of the facial muscles on one side of the face, leading to characteristic symptoms such as drooping of the mouth, difficulty closing one eye, and asymmetry of facial expressions.
In addition to inflammation and compression, ischemia (reduced blood flow) may also contribute to nerve damage in Bell’s palsy. The swelling and edema within the facial canal can compress blood vessels supplying the facial nerve, leading to impaired blood flow and ischemic injury to the nerve fibers.
Overall, the pathophysiology of Bell’s palsy involves a complex interplay of viral infection, inflammation, compression, and ischemia, ultimately resulting in dysfunction of the facial nerve and the characteristic clinical features of the condition. Further research is needed to fully elucidate the underlying mechanisms and identify potential targets for therapeutic intervention. (Nursing Paper Example on Bell’s Palsy: Understanding its Causes, Symptoms, and Management)
DSM-5 Diagnosis
The management of Bell’s palsy aims to alleviate symptoms, promote nerve recovery, and prevent complications. While the condition often resolves spontaneously within a few weeks to months, various treatment options may be considered to expedite recovery and improve outcomes.
- Corticosteroids: Oral corticosteroids, such as prednisone, are commonly prescribed to reduce inflammation and edema of the facial nerve in Bell’s palsy. These medications are typically initiated within the first 72 hours of symptom onset and may be tapered for 10 to 14 days. Corticosteroids have been shown to accelerate recovery and improve facial function in some patients.
- Antiviral Medications: In cases where viral infection is suspected or confirmed, antiviral medications, such as acyclovir or valacyclovir, may be prescribed in combination with corticosteroids. While the evidence supporting the use of antiviral therapy in Bell’s palsy is limited, some studies suggest a potential benefit in certain subsets of patients, particularly those with severe or atypical presentations.
- Eye Care: Patients with Bell’s palsy are at risk of developing corneal exposure and dry eye due to incomplete closure of the affected eye. Lubricating eye drops or ointments may be recommended to prevent corneal abrasions and maintain ocular moisture. In severe cases, temporary eyelid taping or the use of protective eyewear, such as moisture chamber goggles, may be necessary to protect the eye during sleep or daytime activities.
- Physical Therapy: Physical therapy techniques, including facial exercises, massage, and electrical stimulation, may be employed to improve muscle strength, coordination, and mobility in individuals with Bell’s palsy. These interventions can help facilitate nerve regeneration and restore facial function, particularly in cases of incomplete recovery or persistent symptoms.
- Supportive Measures: Patients with Bell’s palsy may benefit from supportive measures to alleviate discomfort and facilitate daily activities. This may include using moist heat packs or gentle massage to relieve facial pain or stiffness, practicing relaxation techniques to reduce stress and anxiety, and modifying dietary habits to accommodate taste disturbances or difficulty chewing. (Nursing Paper Example on Bell’s Palsy: Understanding its Causes, Symptoms, and Management)
Patient Education
Educating patients about Bell’s palsy is essential to promote understanding, compliance with treatment regimens, and optimal self-care. Key aspects of patient education include:
- Nature of the Condition: Providing information about the self-limiting nature of Bell’s palsy and the expected course of recovery, which typically occurs within weeks to months, can help alleviate anxiety and uncertainty.
- Importance of Eye Care: Emphasizing the importance of eye protection and regular eye care, including the use of lubricating eye drops and protective eyewear, to prevent corneal injury and maintain visual health in individuals with incomplete eyelid closure.
- Treatment Goals and Expectations: Discussing treatment options, including the potential benefits and risks of corticosteroids and antiviral medications, and setting realistic expectations regarding the timeline and outcomes of therapy.
- Facial Exercises and Self-Care: Providing guidance on performing facial exercises, practicing good oral hygiene, and implementing supportive measures at home to promote facial muscle strength, mobility, and comfort.
- Follow-Up and Monitoring: Advising patients to follow up with their healthcare provider regularly to monitor progress, assess treatment response, and address any concerns or complications that may arise during treatment.
By empowering patients with knowledge and resources to actively participate in their care, healthcare providers can facilitate better outcomes and enhance the overall management of Bell’s palsy. (Nursing Paper Example on Bell’s Palsy: Understanding its Causes, Symptoms, and Management)



