Comprehensive Nursing Paper Example on Bronchitis: Understanding the Common Respiratory Condition
Comprehensive Nursing Paper Example on Bronchitis: Understanding the Common Respiratory Condition
Causes
Bronchitis can be triggered by various factors, with the most common being viral and bacterial infections. Respiratory viruses such as influenza, rhinovirus, and respiratory syncytial virus (RSV) are frequent culprits, especially during colder months when respiratory illnesses are more prevalent. These viruses invade the respiratory tract, causing inflammation of the bronchial tubes and subsequent bronchitis symptoms.
In addition to infections, exposure to irritants plays a significant role in bronchitis development. Tobacco smoke, whether firsthand or secondhand, is a potent irritant known to inflame the bronchial tubes, leading to acute and chronic bronchitis in smokers and nonsmokers alike. Environmental pollutants, such as air pollution, industrial chemicals, and dust, can also irritate the airways and contribute to bronchitis.
Individual susceptibility to bronchitis varies, with certain risk factors predisposing individuals to the condition. Chronic exposure to irritants like tobacco smoke, air pollution, and occupational hazards increases the likelihood of developing chronic bronchitis. Furthermore, individuals with compromised immune systems, such as the elderly, young children, and those with underlying health conditions, are more susceptible to bronchitis infections.
Moreover, lifestyle factors play a significant role in bronchitis development. Poor hygiene practices, inadequate handwashing, and close contact with infected individuals can facilitate the spread of respiratory viruses, leading to bronchitis outbreaks in communities. Additionally, individuals with weakened immune systems due to factors such as malnutrition, stress, or chronic illnesses are at higher risk of contracting bronchitis.
Overall, bronchitis is a multifactorial condition influenced by various infectious, environmental, and lifestyle factors. Understanding these causes is essential for implementing preventive measures and managing bronchitis effectively, thereby reducing its impact on individuals’ respiratory health and overall well-being. (Comprehensive Nursing Paper Example on Bronchitis: Understanding the Common Respiratory Condition)
Signs and Symptoms
Bronchitis manifests with a range of signs and symptoms that can vary in severity and duration. The most common symptom is a persistent cough, which may be dry initially but often progresses to produce mucus as the condition worsens. This cough is typically accompanied by chest discomfort or tightness, which can range from mild to severe.
Excessive mucus production is a hallmark feature of bronchitis, leading to phlegm or sputum being expelled during coughing episodes. The color and consistency of the mucus can vary, ranging from clear or white to yellow or green, depending on the underlying cause of bronchitis.
In addition to coughing and mucus production, individuals with bronchitis may experience respiratory symptoms such as shortness of breath or wheezing. These symptoms result from inflammation and narrowing of the bronchial tubes, which restrict airflow and impair breathing.
Fatigue and malaise are common systemic symptoms associated with bronchitis, as the body expends energy to fight off the infection or inflammation. Individuals may feel tired or lethargic, with reduced energy levels and overall stamina.
Fever is another possible symptom of bronchitis, particularly in cases caused by bacterial infections. Elevated body temperature indicates an immune response to the underlying infection, although not all individuals with bronchitis will experience fever.
In acute cases of bronchitis, symptoms typically develop suddenly and may resolve within a few weeks with appropriate treatment and supportive care. Chronic bronchitis, on the other hand, is characterized by persistent or recurrent symptoms lasting for months or years, often accompanied by exacerbations or flare-ups.
Overall, recognizing the signs and symptoms of bronchitis is crucial for timely diagnosis and management, as early intervention can help alleviate symptoms, prevent complications, and promote recovery. (Comprehensive Nursing Paper Example on Bronchitis: Understanding the Common Respiratory Condition)
Etiology
Bronchitis can be classified into acute and chronic forms, each with distinct etiological factors contributing to its development.
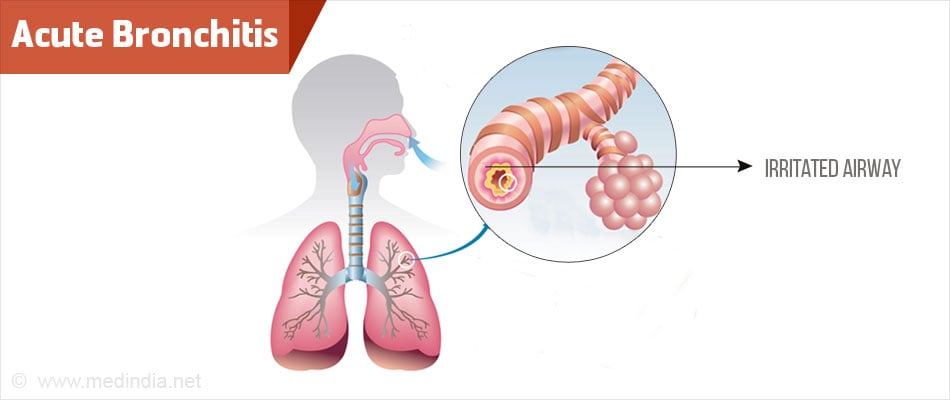
Acute Bronchitis: Acute bronchitis is commonly caused by viral infections, with respiratory viruses such as influenza, rhinovirus, adenovirus, and respiratory syncytial virus (RSV) being the primary culprits. These viruses invade the respiratory tract, infecting the epithelial cells lining the bronchial tubes and triggering an inflammatory response. The resulting inflammation leads to swelling of the bronchial walls and increased mucus production, contributing to the characteristic symptoms of acute bronchitis.
In addition to viral infections, acute bronchitis can also be caused by bacterial infections, although less frequently. Bacterial pathogens such as Mycoplasma pneumoniae, Bordetella pertussis (pertussis), and Streptococcus pneumoniae can infect the bronchial tubes, leading to acute bronchitis with similar symptoms as viral infections.
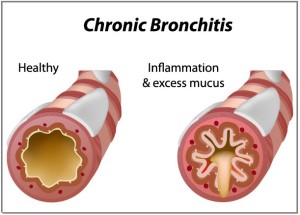
Chronic Bronchitis: Chronic bronchitis is primarily associated with long-term exposure to irritants, particularly tobacco smoke. Smoking is the leading cause of chronic bronchitis, with the toxic chemicals in cigarette smoke irritating the bronchial tubes and causing chronic inflammation. Prolonged exposure to tobacco smoke damages the cilia lining the bronchial tubes, impairing their ability to clear mucus and debris, and leading to mucus buildup and airway obstruction.
In addition to smoking, chronic bronchitis can also be caused by environmental pollutants such as air pollution, occupational exposure to dust and chemicals, and indoor air pollutants. These irritants can exacerbate bronchial inflammation and contribute to the development and progression of chronic bronchitis, particularly in individuals with pre-existing respiratory conditions or genetic predispositions.
Overall, understanding the etiological factors underlying acute and chronic bronchitis is essential for implementing preventive measures and targeted interventions to reduce the burden of this respiratory condition. Efforts to mitigate exposure to respiratory viruses, tobacco smoke, and environmental pollutants are crucial in preventing bronchitis and promoting respiratory health. (Comprehensive Nursing Paper Example on Bronchitis: Understanding the Common Respiratory Condition)
Pathophysiology
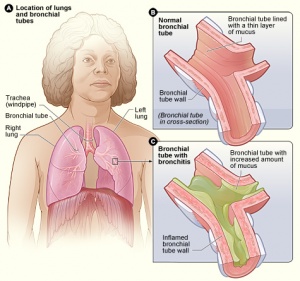
Bronchitis is characterized by inflammation of the bronchial tubes, which play a crucial role in the pathophysiology of the condition. The inflammatory process involves a complex interplay of immune cells, cytokines, and inflammatory mediators, leading to structural changes in the airways and disruption of normal respiratory function.
In response to viral or bacterial infections, the immune system mounts an inflammatory response in the bronchial tubes, characterized by the infiltration of inflammatory cells such as neutrophils, lymphocytes, and macrophages. These cells release pro-inflammatory cytokines and mediators, including interleukins, tumor necrosis factor-alpha (TNF-alpha), and leukotrienes, which contribute to bronchial inflammation and tissue damage.
The inflammatory process results in swelling and edema of the bronchial walls, narrowing the airway lumen and impairing airflow. Additionally, increased mucus production by goblet cells in the bronchial epithelium leads to the accumulation of mucus in the airways, further obstructing airflow and contributing to cough and sputum production.
Chronic exposure to irritants such as tobacco smoke exacerbates the inflammatory response in the bronchial tubes, leading to chronic bronchitis. Prolonged inflammation and tissue damage result in structural changes in the airways, including hypertrophy and hyperplasia of the mucous glands, goblet cell metaplasia, and fibrosis of the bronchial walls. These changes contribute to airway remodeling and irreversible airflow obstruction characteristic of chronic bronchitis.
Overall, the pathophysiology of bronchitis involves a complex interplay of inflammatory processes, immune responses, and structural changes in the bronchial tubes, leading to airflow obstruction, mucus production, and respiratory symptoms. Understanding the underlying mechanisms of bronchitis is crucial for developing targeted therapeutic strategies aimed at alleviating inflammation, improving airway clearance, and promoting respiratory health. (Comprehensive Nursing Paper Example on Bronchitis: Understanding the Common Respiratory Condition)
DSM-5 Diagnosis
Bronchitis, while primarily a medical diagnosis based on clinical signs and symptoms, is not formally classified in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5). However, it is essential to recognize the potential psychological impact of bronchitis on individuals’ mental health and well-being.
Individuals with bronchitis may experience psychological distress due to the physical discomfort and limitations imposed by the condition. Persistent coughing, chest discomfort, shortness of breath, and fatigue can significantly impact daily activities, leading to frustration, anxiety, and depression in some cases.
Moreover, chronic bronchitis, characterized by recurrent or persistent respiratory symptoms lasting for months or years, can have a profound effect on individuals’ quality of life. The chronic nature of the condition, coupled with the potential for exacerbations and flare-ups, may contribute to feelings of hopelessness, helplessness, and social isolation.
Furthermore, bronchitis can exacerbate existing mental health conditions or contribute to the development of new psychiatric symptoms. Individuals with pre-existing anxiety disorders or depression may experience worsening symptoms during bronchitis episodes, while others may develop psychological symptoms in response to the physical and emotional burden of the condition.
Although bronchitis itself is not classified in the DSM-5, healthcare professionals should be aware of the potential psychological impact of the condition and consider screening patients for mental health concerns. Integrating psychological support and counseling into the management of bronchitis can help address emotional distress, improve coping strategies, and enhance overall patient well-being.
While bronchitis is primarily a medical diagnosis, its potential psychological implications highlight the importance of a holistic approach to patient care that addresses both physical and emotional well-being. (Comprehensive Nursing Paper Example on Bronchitis: Understanding the Common Respiratory Condition)
Treatment Regimens and Patient Education
Effective management of bronchitis involves a combination of pharmacological and non-pharmacological interventions aimed at alleviating symptoms, promoting recovery, and preventing complications. Additionally, patient education plays a crucial role in empowering individuals to manage their condition effectively and adopt healthy lifestyle behaviors.
Pharmacological Interventions:
- Analgesics and Antipyretics: Over-the-counter pain relievers such as acetaminophen or ibuprofen may be recommended to alleviate chest discomfort and reduce fever associated with bronchitis.
- Cough Suppressants: Cough suppressants, such as dextromethorphan, can help reduce the frequency and intensity of coughing episodes, providing symptomatic relief.
- Expectorants: Expectorants, such as guaifenesin, help thin and loosen mucus, making it easier to expel from the airways during coughing.
- Bronchodilators: In cases of bronchitis with significant airway obstruction or wheezing, bronchodilators such as albuterol may be prescribed to relax the bronchial muscles and improve airflow.
- Antibiotics: Antibiotics are not routinely recommended for acute bronchitis caused by viral infections. However, in cases of bacterial bronchitis or secondary bacterial infections, antibiotics may be prescribed to target the underlying bacterial pathogens.
Non-Pharmacological Interventions:
- Rest and Hydration: Adequate rest and hydration are essential for supporting the body’s immune response and promoting recovery from bronchitis. Patients should be advised to get plenty of rest and drink fluids to stay hydrated.
- Humidifiers: Using a humidifier or steam inhalation can help soothe irritated airways and alleviate coughing and congestion by adding moisture to the air.
- Smoking Cessation: For individuals with chronic bronchitis or a history of smoking, smoking cessation is crucial to prevent further damage to the respiratory system and improve long-term outcomes.
- Avoidance of Irritants: Patients should be educated about avoiding exposure to tobacco smoke, air pollution, and other respiratory irritants that can exacerbate bronchitis symptoms and worsen respiratory function.
- Hand Hygiene: Practicing good hand hygiene, including frequent handwashing with soap and water, can help prevent the spread of respiratory viruses and reduce the risk of bronchitis infections.
Patient Education:
- Understanding Bronchitis: Patients should be educated about the causes, signs, and symptoms of bronchitis to help them recognize and manage the condition effectively.
- Medication Adherence: It is essential to educate patients about the proper use of prescribed medications, including dosage, frequency, and potential side effects.
- Lifestyle Modifications: Encouraging patients to adopt a healthy lifestyle, including regular exercise, balanced nutrition, and smoking cessation, can help improve respiratory health and reduce the risk of recurrent bronchitis episodes.
- Recognizing Complications: Patients should be informed about the potential complications of bronchitis, such as pneumonia or exacerbations of underlying respiratory conditions, and when to seek medical attention.
- Follow-Up Care: Patients should be advised to follow up with their healthcare provider for monitoring and management of bronchitis, especially in cases of chronic or recurrent symptoms.
The treatment of bronchitis involves a combination of pharmacological and non-pharmacological interventions tailored to individual patient needs. Patient education is crucial for empowering individuals to manage their condition effectively, prevent complications, and promote respiratory health and overall well-being. (Comprehensive Nursing Paper Example on Bronchitis: Understanding the Common Respiratory Condition)