Nursing Paper Example on Bruxism: Understanding the Grind
Nursing Paper Example on Bruxism: Understanding the Grind
Causes
Bruxism, characterized by the rhythmic clenching or grinding of teeth, is influenced by a myriad of factors, both intrinsic and extrinsic. One prominent contributor to bruxism is psychological stress and anxiety. Individuals experiencing heightened levels of stress often exhibit increased muscle tension, including the muscles involved in jaw movement, leading to bruxism episodes during sleep. Additionally, malocclusion, or misalignment of the teeth and jaw, can predispose individuals to bruxism. The irregular contact between teeth due to misalignment may prompt subconscious efforts to adjust the bite, resulting in grinding or clenching.
Lifestyle habits also play a significant role in the development and exacerbation of bruxism. Consumption of stimulants such as caffeine and nicotine can heighten arousal levels, potentially intensifying bruxism episodes. Furthermore, alcohol consumption has been associated with increased bruxism frequency, likely due to its sedative effects on the central nervous system, leading to disrupted sleep patterns.
Moreover, bruxism has been linked to certain medications and medical conditions. Psychiatric medications, particularly selective serotonin reuptake inhibitors (SSRIs) and dopamine agonists, have been implicated in inducing or exacerbating bruxism as a side effect. Additionally, neurological disorders such as Parkinson’s disease and Huntington’s disease are often accompanied by bruxism as a secondary symptom.
Genetic predispositions may also contribute to the development of bruxism. Research suggests that variations in genes related to neurotransmitter regulation and muscle function may increase susceptibility to bruxism. Family history of bruxism may therefore serve as a predisposing factor, although further studies are warranted to elucidate the precise genetic mechanisms involved.
In summary, bruxism arises from a complex interplay of psychological, physiological, and environmental factors. Understanding these diverse causes is crucial for implementing targeted interventions aimed at alleviating bruxism symptoms and improving overall patient well-being. (Nursing Paper Example on Bruxism: Understanding the Grind)
Signs and Symptoms
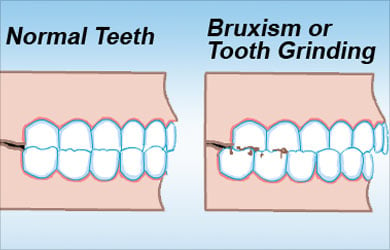
Bruxism, while often occurring unconsciously during sleep, manifests through various signs and symptoms that can significantly impact an individual’s oral health and overall well-being. One of the hallmark signs of bruxism is tooth wear, characterized by the gradual erosion of tooth enamel due to repetitive grinding or clenching. This can lead to tooth sensitivity, increased risk of dental decay, and eventual tooth loss if left untreated.
Facial pain and headaches are common symptoms experienced by individuals with bruxism. The constant strain placed on the jaw muscles during grinding or clenching can result in temporomandibular joint (TMJ) discomfort, facial muscle fatigue, and tension headaches. This discomfort may extend to the ears, manifesting as earaches or ringing in the ears (tinnitus).
Additionally, individuals with bruxism often report jaw stiffness and difficulty opening or closing their mouths fully, particularly upon waking in the morning. This limitation in jaw mobility, known as trismus, can interfere with daily activities such as eating and speaking, impacting the individual’s quality of life.
Disturbed sleep patterns are another common symptom associated with bruxism. The repetitive movements of grinding or clenching can disrupt normal sleep cycles, leading to frequent awakenings throughout the night. Consequently, individuals may experience daytime fatigue, irritability, and difficulty concentrating due to insufficient restorative sleep.
Furthermore, bruxism can have aesthetic implications, as excessive grinding or clenching may cause changes in facial appearance. These changes can include hypertrophy of the jaw muscles, asymmetry of the face, and accelerated aging of the teeth due to wear and tear.
Overall, recognizing the signs and symptoms of bruxism is essential for early intervention and effective management to prevent further oral complications and improve the individual’s quality of life. (Nursing Paper Example on Bruxism: Understanding the Grind)
Etiology
Pathophysiology
Bruxism, characterized by the involuntary clenching or grinding of teeth, involves intricate neuromuscular mechanisms influenced by both central and peripheral factors. Dysfunction in neurotransmitter regulation within the central nervous system (CNS) contributes to the pathophysiology of bruxism. Specifically, alterations in the levels of neurotransmitters such as serotonin, dopamine, and norepinephrine may disrupt the balance between excitatory and inhibitory signals, leading to hyperactivity of the masticatory muscles involved in jaw movement.
Peripheral factors, including sensory processing and muscle function, also play a crucial role in the pathophysiology of bruxism. Individuals with bruxism often exhibit heightened sensory responses, characterized by increased sensitivity to oral stimuli. This heightened sensory processing may contribute to the exaggerated muscle activity observed during grinding or clenching episodes.
Furthermore, structural abnormalities within the temporomandibular joint (TMJ) and surrounding musculature can exacerbate bruxism symptoms. Malocclusion, or misalignment of the teeth and jaw, creates irregular contact between dental surfaces, prompting compensatory adjustments in jaw position and muscle activity to achieve a stable bite. These repetitive adjustments can lead to muscle fatigue, pain, and ultimately, the development of bruxism.
Moreover, psychological factors such as stress and anxiety can influence the pathophysiology of bruxism through their effects on CNS neurotransmitter activity and muscle tension. Heightened levels of stress can trigger an exaggerated stress response, leading to increased muscle tension and hyperactivity within the masticatory system.
In summary, bruxism involves a complex interplay of central and peripheral factors, including altered neurotransmitter regulation, heightened sensory processing, and structural abnormalities within the TMJ and surrounding musculature. Understanding these underlying mechanisms is crucial for developing targeted interventions to alleviate bruxism symptoms and improve patient outcomes. (Nursing Paper Example on Bruxism: Understanding the Grind)
DMS-5 Diagnosis
Treatment Regimens and Patient Education
Effective management of bruxism involves a comprehensive approach that combines therapeutic interventions with patient education to address both the underlying causes and symptoms of the condition.
Treatment Regimens:
- Behavioral Interventions: Behavioral therapies focus on identifying and managing stressors that contribute to bruxism. Stress management techniques such as relaxation exercises, mindfulness meditation, and cognitive-behavioral therapy (CBT) can help individuals reduce anxiety levels and alleviate bruxism-related symptoms.
- Oral Appliances: Custom-made mouthguards or splints, also known as occlusal guards or bite splints, are commonly prescribed to individuals with bruxism. These oral appliances are designed to protect the teeth from grinding or clenching forces and promote a more relaxed jaw position during sleep.
- Medications: In certain cases, medications may be prescribed to alleviate bruxism symptoms. Muscle relaxants, such as benzodiazepines or cyclobenzaprine, can help reduce muscle tension and prevent grinding or clenching activity during sleep. Additionally, antidepressants or anti-anxiety medications may be prescribed to manage underlying psychological factors contributing to bruxism.
- Dental Procedures: Dental treatments such as occlusal adjustments, dental restorations, and orthodontic interventions may be recommended to correct malocclusion and restore proper dental alignment. These procedures aim to eliminate dental abnormalities that contribute to bruxism and alleviate associated symptoms.
Patient Education:
- Awareness and Monitoring: Educating patients about the signs and symptoms of bruxism is essential for early detection and intervention. Encouraging individuals to monitor their oral habits, such as teeth clenching or grinding during the day, can help raise awareness of the condition and prompt timely intervention.
- Stress Management Techniques: Teaching stress management techniques, such as deep breathing exercises, progressive muscle relaxation, and mindfulness practices, empowers patients to proactively manage stress and reduce its impact on bruxism symptoms.
- Oral Hygiene Practices: Emphasizing the importance of maintaining good oral hygiene practices, including regular brushing, flossing, and dental check-ups, is crucial for preventing dental complications associated with bruxism, such as tooth wear and decay.
- Lifestyle Modifications: Educating patients about lifestyle modifications, such as reducing caffeine and alcohol consumption, practicing good sleep hygiene, and avoiding chewing on hard objects, can help minimize triggers and exacerbating factors for bruxism.
By combining treatment regimens with comprehensive patient education, clinicians can empower individuals with bruxism to actively participate in their care and achieve improved management of the condition, ultimately enhancing their oral health and overall well-being. (Nursing Paper Example on Bruxism: Understanding the Grind)
Conclusion
Bruxism, characterized by the involuntary grinding or clenching of teeth, presents a multifaceted challenge requiring a comprehensive approach for effective management. Understanding the causes, signs and symptoms, etiology, pathophysiology, DSM-5 diagnosis, treatment regimens, and patient education is crucial in addressing this prevalent condition. By exploring the intricate interplay of psychological, physiological, and environmental factors contributing to bruxism, clinicians can tailor treatment regimens to alleviate symptoms and improve patient outcomes. Incorporating behavioral interventions, oral appliances, medications, and dental procedures, alongside comprehensive patient education on stress management, oral hygiene practices, and lifestyle modifications, empowers individuals to actively participate in their care. Through proactive management strategies and ongoing patient education, clinicians can mitigate the adverse effects of bruxism, preserve oral health, and enhance overall quality of life for affected individuals. A holistic approach that addresses both the underlying causes and symptoms of bruxism is essential for achieving optimal outcomes and promoting long-term oral well-being. (Nursing Paper Example on Bruxism: Understanding the Grind)
References
https://www.ncbi.nlm.nih.gov/books/NBK482466/



