Nursing Paper Example on Strabismus
Nursing Paper Example on Strabismus
Strabismus, commonly referred to as “crossed eyes” or “squint,” is a visual disorder where the eyes are misaligned and point in different directions. This misalignment can lead to various vision issues, as the eyes fail to work together to focus on the same object. Strabismus affects people of all ages but is most common in children. Early diagnosis and treatment are essential to prevent complications like amblyopia or “lazy eye.” This overview will explore the causes, types, pathophysiology, signs and symptoms, diagnostic methods, and treatment options for strabismus.
Causes and Pathophysiology
Primary Causes
Strabismus results from an imbalance in the eye muscles, an issue with the nerves transmitting information to these muscles, or problems within the brain responsible for coordinating eye movements. The disorder can be congenital, often due to genetics, or acquired through conditions such as stroke, traumatic brain injury, or neurological issues. In children, refractive errors like farsightedness can also lead to strabismus as the eye muscles strain to focus (Holmes & Clarke, 2006).
Pathophysiology
Strabismus arises when the eyes fail to maintain alignment due to weakened or overactive eye muscles. Six muscles control eye movement, allowing for up, down, side, and rotational motions. In healthy eyes, these muscles coordinate for both eyes to focus on a single point. However, with strabismus, one or more muscles may be underactive or overactive, causing the affected eye to deviate. Over time, the brain may ignore input from the misaligned eye to avoid double vision, which can result in amblyopia (Scott & Mashige, 2016).
(Nursing Paper Example on Strabismus)
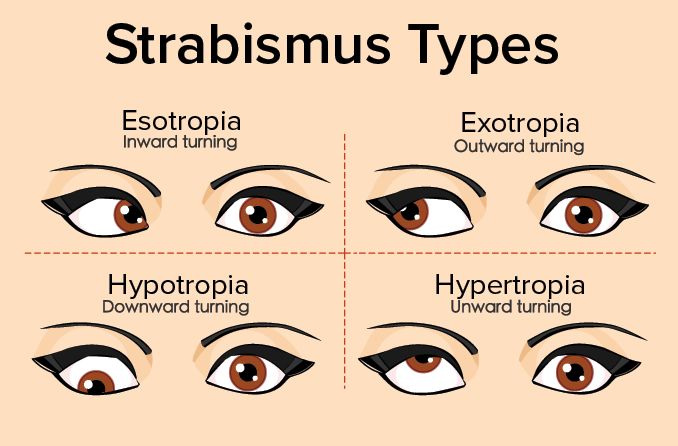
Types of Strabismus
Esotropia
Esotropia occurs when one or both eyes turn inward. It is the most common type of strabismus in infants and can be constant or intermittent. Esotropia is often related to congenital issues or neurological conditions (Burian, 2015).
Exotropia
Exotropia, or “wall-eye,” is characterized by outward deviation of the eye. It may be present intermittently, often during times of tiredness or when focusing on distant objects. Exotropia is more common in older children and adults than in infants (Holmes & Clarke, 2006).
Hypertropia and Hypotropia
In hypertropia, the eye turns upward, while hypotropia involves downward turning. These types of vertical strabismus are less common but may indicate a neurological disorder or be associated with congenital abnormalities (Scott & Mashige, 2016).
Signs and Symptoms
Individuals with strabismus may experience several symptoms, which vary based on the severity and type of strabismus.
Primary Symptoms
Common symptoms include:
- Eyes pointing in different directions
- Double vision (diplopia)
- Frequent squinting or closing one eye, especially in bright light
- Head tilting to improve focus
In Children
Children may exhibit symptoms such as misaligned eyes, frequent eye rubbing, or lack of depth perception. Untreated strabismus in children often leads to amblyopia, as the brain suppresses images from the misaligned eye (Burian, 2015).
Diagnosis
Eye Examination
An ophthalmologist or optometrist diagnoses strabismus through a comprehensive eye exam. The Hirschberg test (corneal light reflex test) and cover test are commonly used to evaluate eye alignment and identify the type of strabismus.
Visual Acuity and Refraction Tests
These tests help assess the sharpness of vision and any refractive errors contributing to strabismus. Hyperopia, or farsightedness, is often associated with strabismus in children (Scott & Mashige, 2016).
Neurological Assessment
In cases where strabismus arises suddenly in adults, a neurological exam may be necessary to rule out serious conditions like brain tumors, stroke, or head trauma. Imaging studies, such as MRI or CT scans, can be employed if a neurological cause is suspected.
(Nursing Paper Example on Strabismus)
Treatment and Management
Corrective Lenses
For strabismus associated with refractive errors, prescription glasses or contact lenses can improve focus and alignment. Prism lenses are sometimes used to alter the light entering the eye, helping reduce double vision (Holmes & Clarke, 2006).
Vision Therapy
Vision therapy is often effective for certain types of strabismus, particularly for intermittent or mild forms. It involves exercises to strengthen eye muscles, improve coordination, and enhance depth perception.
Surgical Intervention
Eye muscle surgery is the primary treatment for severe or persistent strabismus. Surgeons adjust the position or length of eye muscles to achieve proper alignment. The procedure is commonly performed on children but may also be effective for adults. While surgery often improves alignment, it may not restore perfect depth perception, and follow-up treatments may be necessary (Burian, 2015).
Botulinum Toxin (Botox) Injections
Botulinum toxin injections may be used as a non-surgical option to temporarily weaken overactive eye muscles, particularly in adults with acquired strabismus. Botox is typically considered when surgery is not an option or as a temporary solution (Scott & Mashige, 2016).
Complications and Prognosis
Untreated strabismus, especially in children, can lead to amblyopia or permanent vision loss in the misaligned eye. Early diagnosis and treatment are essential to prevent these complications. In adults, untreated strabismus may lead to chronic double vision, impacting daily life and quality of life.
While children respond well to treatment, adults may experience limited success with certain interventions due to established neural pathways. However, with appropriate management, strabismus can be effectively controlled, reducing symptoms and improving visual alignment.
Conclusion
Strabismus is a complex eye condition that can significantly affect vision and quality of life if left untreated. With varied causes, including genetics, neurological factors, and refractive errors, it requires a multi-faceted approach for effective management. Treatment options range from corrective lenses and vision therapy to surgery and Botox injections, depending on the type and severity of the condition. Early intervention, especially in children, is key to preventing complications like amblyopia and preserving normal vision. For adults, treatment options remain available, although results may vary.
References
Burian, H. M. (2015). Pediatric Strabismus and Amblyopia. Journal of Pediatric Ophthalmology and Strabismus, 52(1), 23-30. https://journals.healio.com/journal/jpos
Holmes, J. M., & Clarke, M. P. (2006). Amblyopia. The Lancet, 367(9519), 1343-1351. https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(06)68581-3/fulltext
Scott, W. E., & Mashige, K. P. (2016). Clinical management of strabismus in children and adults. Clinical Eye and Vision Care, 9(4), 233-246. https://www.sciencedirect.com/science/article/abs/pii/S0959270916000209


