Ensuring Healthcare Access
Ensuring Healthcare Access
Introduction
In the realm of healthcare, the Medicare insurance program stands as a cornerstone, providing vital coverage for millions of Americans. Established in 1965, Medicare was designed to address the healthcare needs of individuals aged 65 and older. Over the years, it has evolved to encompass broader demographic groups, playing a pivotal role in shaping the landscape of healthcare access in the United States.
Background
The origin of the Medicare insurance program traces back to a critical juncture in American history, marked by a pressing need for comprehensive healthcare coverage for the elderly. In the early 1960s, as medical advancements increased life expectancy, a significant portion of the population found itself grappling with the financial strain of accessing essential healthcare services. With seniors facing mounting healthcare costs, policymakers recognized the imperative to intervene and establish a safety net.

In 1965, the Medicare program emerged as a response to this pressing need. President Lyndon B. Johnson signed the Social Security Amendments into law, ushering in a new era of healthcare access for the elderly and, subsequently, for individuals with certain disabilities. The primary objective was to ensure that seniors, who had contributed to the nation throughout their working lives, could age with dignity and without the looming specter of financial ruin due to medical expenses.
Initially, Medicare comprised two parts: Part A, addressing hospital insurance, and Part B, focusing on medical insurance. Part A predominantly covered hospital stays, skilled nursing facility care, and some home health services. On the other hand, Part B included outpatient care, preventive services, and durable medical equipment. This bifurcation laid the groundwork for a comprehensive approach to healthcare, acknowledging the diverse needs of the aging population.
Over the years, Medicare underwent several expansions and revisions to keep pace with the evolving healthcare landscape. Notably, in 1972, Medicare eligibility was extended to individuals under 65 with long-term disabilities and those suffering from end-stage renal disease. These amendments broadened the program’s scope, emphasizing inclusivity and recognizing that healthcare needs transcend age.
The 1980s witnessed further enhancements with the addition of Medicare Part C, known as Medicare Advantage, allowing beneficiaries to opt for private health plans. Subsequently, in 2003, Part D was introduced to address the crucial realm of prescription drug coverage. These additions were strategic responses to the changing dynamics of healthcare demands, reflecting a commitment to adaptability and relevance.
The significance of Medicare is not confined to its immediate beneficiaries; it reverberates across the entire healthcare ecosystem. As a federal program, Medicare operates in tandem with private insurance options, creating a dynamic interplay that defines the contours of the nation’s healthcare framework. The program’s role as a safety net resonates beyond its beneficiaries, influencing healthcare providers’ practices and contributing to ongoing dialogues about healthcare reform.
Moreover, Medicare’s existence shapes the standards for reimbursement rates, positioning it as a formidable force in negotiating acceptable levels of care. This has profound implications for both providers and beneficiaries, creating a symbiotic relationship that balances quality care with financial sustainability.
In essence, the background of Medicare embodies a narrative of compassion, foresight, and adaptability. What began as a targeted solution for the elderly has evolved into a comprehensive program that caters to a diverse demographic, underscoring the nation’s commitment to equitable healthcare access. As we navigate the intricate layers of Medicare’s evolution, it becomes apparent that its foundation is rooted in a fundamental belief – that healthcare is a right, not a privilege, and that every American deserves a pathway to well-being, regardless of age or circumstance.
Role of Medicare
The role of the Medicare insurance program is pivotal, serving as a bedrock for healthcare accessibility in the United States. Established in 1965, Medicare’s primary objective is to provide comprehensive coverage for medical services to individuals aged 65 and older. Over time, its role has expanded, encompassing a broader demographic and addressing diverse healthcare needs.
At its core, Medicare functions as a safety net, offering coverage for a spectrum of medical services crucial for maintaining health and well-being. Part A, focusing on hospital insurance, ensures that beneficiaries have access to inpatient care, skilled nursing facilities, and essential home health services. Simultaneously, Part B, the medical insurance component, covers outpatient care, preventive services, and durable medical equipment, creating a comprehensive approach to healthcare.
Medicare’s significance extends beyond its direct impact on beneficiaries. As a federal program, it coexists with private insurance options, contributing to the complex tapestry of the nation’s healthcare framework. Its role as a payer with substantial negotiating power shapes reimbursement rates and sets standards for acceptable levels of care. This influence, in turn, fosters a balance between quality healthcare and financial sustainability.
The program’s adaptability is evident in its response to the changing landscape of healthcare demands. Recognizing the need for flexibility, Medicare introduced Part C, known as Medicare Advantage, in the 1980s. This allowed beneficiaries to opt for private health plans, adding a layer of choice to the program. Subsequently, in 2003, the introduction of Part D addressed the critical realm of prescription drug coverage, ensuring a more holistic approach to healthcare services.
Medicare’s role extends to influencing the practices of healthcare providers across the nation. As a significant payer, it establishes benchmarks for acceptable levels of care, fostering a commitment to high-quality healthcare delivery. Providers, in turn, adapt their practices to align with these standards, creating a symbiotic relationship that benefits both the healthcare system and its beneficiaries.
Importantly, the role of Medicare in healthcare access goes beyond individual beneficiaries. It has a profound impact on the broader healthcare landscape, contributing to ongoing discussions about healthcare reform. Its existence prompts conversations about the balance between public and private healthcare entities, seeking ways to enhance efficiency and coordination in care delivery.
In essence, the role of Medicare is multifaceted and dynamic. It is a lifeline for millions, ensuring that they can access necessary medical services without facing insurmountable financial barriers. Simultaneously, it serves as a benchmark, shaping the standards of care and influencing the practices of healthcare providers. As the nation continues to navigate the complexities of healthcare, Medicare remains a stalwart force, upholding the principles of accessibility, affordability, and quality care for all. (Ensuring Healthcare Access)
Parts of Medicare
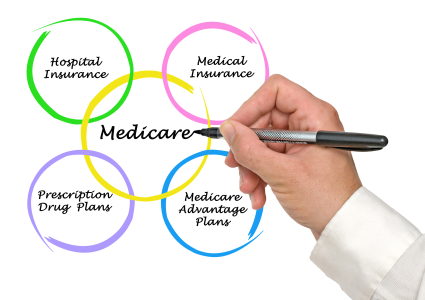
Medicare, the cornerstone of American healthcare, is organized into distinct parts, each addressing specific facets of healthcare needs. This segmentation ensures a comprehensive approach to coverage, catering to the diverse requirements of beneficiaries.

Part A, often referred to as hospital insurance, is foundational. It covers inpatient hospital stays, skilled nursing facility care, and certain home health services. This component lays the groundwork for addressing critical medical needs that necessitate hospitalization, ensuring that beneficiaries have financial protection during such events.
Complementing Part A is Part B, known as medical insurance. This segment encompasses outpatient care, preventive services, and durable medical equipment. By extending coverage to medical services outside the hospital setting, Part B ensures a holistic approach to healthcare. Preventive services play a crucial role in maintaining overall health and well-being.
In the landscape of Medicare, Part C, or Medicare Advantage, adds a layer of choice and flexibility. Introduced in the 1980s, this option allows beneficiaries to opt for private health plans. Medicare Advantage plans often include additional benefits beyond the scope of Parts A and B, such as vision and dental coverage, contributing to a more comprehensive healthcare package.
The introduction of Part D in 2003 addressed a critical gap in coverage—prescription drugs. Part D focuses exclusively on providing coverage for prescription medications, acknowledging the escalating costs of pharmaceuticals, and ensuring that beneficiaries have access to necessary medications without facing exorbitant out-of-pocket expenses.
The segmentation of Medicare into distinct parts aligns with the program’s commitment to addressing the multifaceted nature of healthcare needs. Each part plays a unique and complementary role, collectively forming a robust safety net for beneficiaries. As individuals navigate the complexities of healthcare, the segmentation of Medicare into Parts A, B, C, and D provides a roadmap, ensuring that coverage extends to various aspects of medical care, from hospital stays to prescription medications. This structure not only enhances the comprehensiveness of the program but also underscores its adaptability to the evolving landscape of healthcare demands.
The parts of Medicare function synergistically to provide a comprehensive and adaptable healthcare coverage framework. From foundational hospital insurance to medical services outside hospital walls, and from the flexibility offered by Medicare Advantage to the critical coverage of prescription drugs, each part contributes to the overarching goal of ensuring that beneficiaries can access the necessary care without undue financial burden. This segmentation embodies the program’s commitment to meeting the diverse needs of its beneficiaries, encapsulating the principles of accessibility, affordability, and quality healthcare for all. (Ensuring Healthcare Access)
Eligibility for Medicare
Understanding Medicare eligibility is crucial for individuals seeking access to this vital healthcare program. The primary pathway to eligibility is age-based, with individuals becoming eligible at 65, aligning with the traditional retirement age. This age criterion reflects the initial focus of Medicare on addressing the healthcare needs of seniors, acknowledging the increased medical requirements associated with aging.
Beyond age, individuals under 65 can qualify for Medicare based on certain circumstances. Those with specific disabilities, qualifying for Social Security Disability Insurance (SSDI), gain access to Medicare before reaching the traditional age threshold. This provision recognizes the unique healthcare challenges faced by individuals with disabilities, ensuring they have comprehensive coverage when needed.
Furthermore, individuals suffering from specific medical conditions, such as end-stage renal disease (ESRD) or amyotrophic lateral sclerosis (ALS), qualify for Medicare, regardless of age. This approach ensures that individuals facing severe medical conditions have timely access to necessary healthcare services, emphasizing the program’s commitment to inclusivity.
Enrollment in Medicare is not automatic; individuals must actively apply during designated enrollment periods. Familiarity with these periods, including the Initial Enrollment Period and Special Enrollment Periods, is essential to ensure timely access to the benefits of the program.
The implications of Medicare eligibility extend beyond the individual, influencing family dynamics and caregiving responsibilities. Spouses may become eligible based on their partner’s work history, providing coverage options for those who may not qualify on their own. This interconnected approach recognizes the broader health needs of families and reinforces the inclusive nature of the Medicare program.
Medicare eligibility goes beyond age, encompassing disabilities and specific medical conditions. It strives to be inclusive, ensuring that all eligible individuals, regardless of age or circumstance, can access comprehensive healthcare coverage. Understanding the nuances of eligibility is key, empowering individuals to navigate the process and avail themselves of the benefits offered by Medicare when needed.
How Medicare Affects Healthcare Access
Medicare, as a safety net, profoundly impacts healthcare access by alleviating financial barriers for its beneficiaries. Covering a wide array of medical services, from hospital stays to outpatient care and prescription drugs, Medicare ensures that individuals can seek and receive necessary care without facing overwhelming financial burdens.
For seniors, Medicare is particularly crucial as it addresses the heightened healthcare needs associated with aging. It provides a sense of security, allowing them to access essential services without fear of exorbitant costs. The coverage of preventive services also plays a pivotal role in maintaining overall well-being, promoting a proactive approach to healthcare.
Moreover, the influence of Medicare extends beyond individual beneficiaries to shape the broader healthcare landscape. As a substantial payer, Medicare sets standards for reimbursement rates, influencing the practices of healthcare providers. This impact contributes to the ongoing dialogue about healthcare reform, emphasizing the need for a balance between quality care and financial sustainability.
The program’s role in negotiating acceptable levels of care contributes to a harmonious relationship between providers and beneficiaries. Healthcare providers, recognizing Medicare’s influence, often align their practices with the program’s standards, ensuring a consistent and high-quality approach to healthcare delivery.
Despite its significant impact, Medicare is not without challenges. Gaps in coverage, such as dental and vision care, remain, underscoring the need for ongoing improvements. Addressing these gaps and exploring innovative ways to control rising healthcare costs can further enhance the program’s effectiveness in ensuring widespread, affordable, and high-quality healthcare access.
Medicare stands as a linchpin in the realm of healthcare access, alleviating financial burdens for millions of Americans. Its coverage not only supports individual beneficiaries but also shapes the practices of healthcare providers, contributing to the ongoing conversation about healthcare reform. As the healthcare landscape evolves, continuous efforts to improve and refine Medicare will be crucial in maintaining its effectiveness and ensuring equitable access to healthcare services. (Ensuring Healthcare Access)
Potential Changes to Improve Medicare
In the pursuit of refining healthcare access, potential changes to the Medicare program merit consideration. One avenue for improvement involves addressing existing gaps in coverage. Dental and vision care, currently not included in the standard Medicare package, represent critical aspects of overall health. Expanding coverage to encompass these areas would contribute significantly to the program’s comprehensiveness.
Furthermore, exploring innovative strategies to control escalating healthcare costs is paramount. Implementing preventive measures and promoting healthier lifestyles can mitigate the demand for medical services, fostering a more sustainable approach. Such preventive initiatives can be instrumental in reducing the overall burden on the healthcare system while improving the well-being of beneficiaries.
Collaboration between public and private healthcare entities holds promise as well. Fostering synergy between these sectors can lead to more efficient and coordinated care delivery. By leveraging the strengths of both, a unified approach to healthcare can emerge, benefitting Medicare beneficiaries and the healthcare system at large.
Additionally, embracing advancements in technology and telehealth can enhance the accessibility and efficiency of healthcare services. Telehealth, in particular, has demonstrated its potential to expand its reach, especially in remote or underserved areas. Integrating these technological solutions into the Medicare framework can create a more responsive and patient-centric healthcare system.
Strategic changes in reimbursement models can incentivize providers to focus on preventive care and patient outcomes. Shifting from fee-for-service to value-based reimbursement models encourages a proactive approach to healthcare, aligning provider incentives with the overall well-being of Medicare beneficiaries.
Moreover, streamlining administrative processes within the Medicare program can reduce bureaucratic complexities. Simplifying enrollment procedures and enhancing communication channels can make it easier for beneficiaries to navigate the system, ensuring that they receive timely and effective healthcare coverage.
Potential changes to improve Medicare encompass a spectrum of strategies, from addressing coverage gaps to embracing technological advancements. By fostering collaboration, incentivizing preventive care, and streamlining administrative processes, Medicare can evolve to meet the dynamic healthcare landscape. These changes, collectively implemented, hold the promise of enhancing the program’s effectiveness, ensuring that it continues to play a pivotal role in providing accessible, affordable, and high-quality healthcare for all eligible individuals.
Conclusion
Medicare stands poised for transformative improvements. By addressing coverage gaps, embracing preventive measures, and fostering collaboration between public and private sectors, the program can evolve to meet the dynamic needs of its beneficiaries. The expansion to include dental and vision care acknowledges the holistic nature of health, while innovative strategies to control costs and technology integration promise a more efficient and patient-centric system. Streamlining administrative processes and shifting reimbursement models towards value-based care underscore a commitment to adaptability and improvement. As the healthcare landscape continues to evolve, these potential changes signify a dedication to ensuring Medicare remains a dynamic force, providing equitable, accessible, and high-quality healthcare for all eligible individuals. (Ensuring Healthcare Access)
References
Centers for Medicare & Medicaid Services. (n.d.). Medicare.gov. Retrieved from https://www.medicare.gov/
Kaiser Family Foundation. (n.d.). Medicare. Retrieved from https://www.kff.org/medicare/


