Nursing Paper Example on Epilepsy: Causes, Symptoms, Diagnosis, and Treatment [SOLVED]
Nursing Paper Example on Epilepsy: Causes, Symptoms, Diagnosis, and Treatment [SOLVED]
Causes
Epilepsy, a complex neurological disorder, arises from a myriad of underlying causes, ranging from genetic predispositions to acquired brain injuries. Genetic factors play a significant role in epilepsy etiology, with various gene mutations implicated in seizure susceptibility. Mutations affecting ion channels, neurotransmitter receptors, and synaptic proteins disrupt normal neuronal function, leading to hyperexcitability and seizure generation. Moreover, genetic syndromes such as Dravet syndrome, Rett syndrome, and tuberous sclerosis are associated with an increased risk of epilepsy.
Acquired brain injuries represent another common cause of epilepsy, encompassing traumatic brain injuries (TBIs), strokes, brain tumors, and infections. TBIs, resulting from falls, accidents, or assaults, disrupt neuronal integrity and may lead to chronic epilepsy years after the initial injury. Similarly, strokes, caused by cerebral ischemia or hemorrhage, can result in focal brain damage and subsequent seizure activity. Brain tumors, although less common, can exert mass effect on surrounding brain tissue, triggering seizures through compression or infiltration of epileptogenic areas. Additionally, infections such as meningitis, encephalitis, and neurocysticercosis can directly affect brain function, leading to inflammatory responses and neuronal hyperexcitability.
Developmental abnormalities in brain structure or connectivity represent another significant cause of epilepsy. Prenatal insults such as maternal infections, intrauterine trauma, or exposure to teratogenic substances can disrupt normal brain development, predisposing individuals to epilepsy later in life. Furthermore, metabolic disorders, neurodegenerative diseases, and autoimmune conditions may also contribute to epilepsy etiology through various mechanisms, highlighting the diverse array of factors involved in its pathogenesis. Understanding these underlying causes is essential for accurate diagnosis, personalized treatment approaches, and prognostic assessment in individuals with epilepsy. (Nursing Paper Example on Epilepsy: Causes, Symptoms, Diagnosis, and Treatment [SOLVED])
Signs and Symptoms
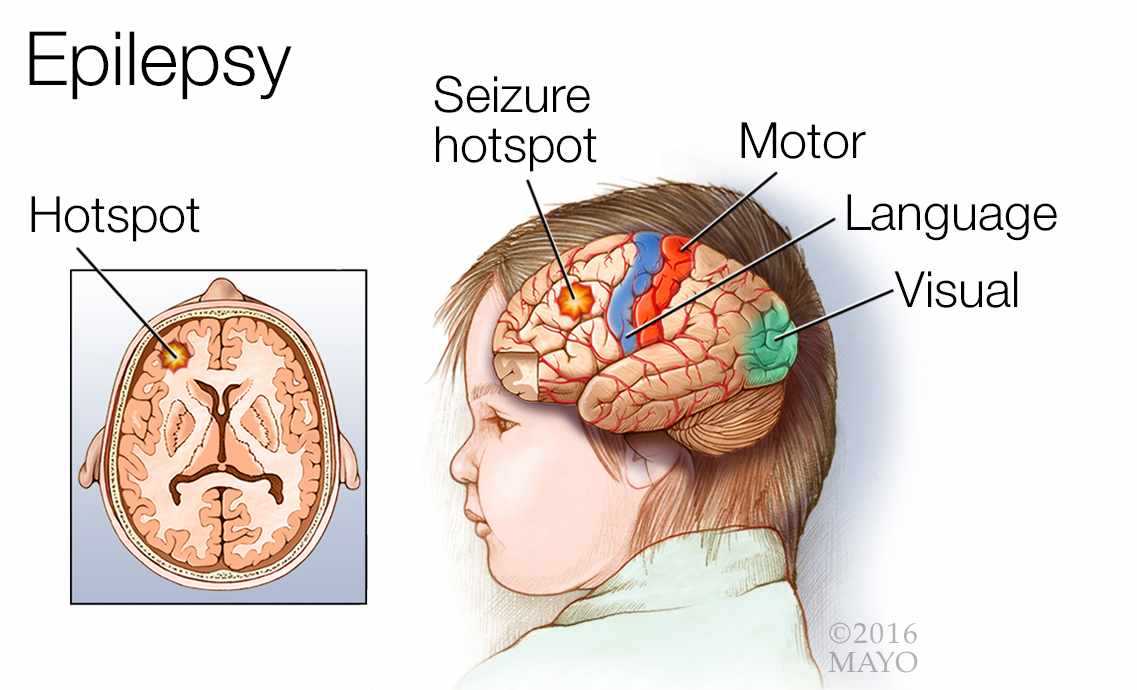
Epilepsy presents a diverse array of signs and symptoms, varying in intensity and manifestation. The hallmark of epilepsy is recurrent seizures, which can manifest in various forms, each carrying its own distinct set of symptoms. Focal seizures, also known as partial seizures, originate in a specific area of the brain and may involve motor, sensory, or emotional disturbances. These seizures can manifest as jerking movements, tingling sensations, or intense emotions, depending on the affected brain region.
Generalized seizures, on the other hand, involve widespread abnormal neuronal activity throughout the brain, resulting in loss of consciousness and dramatic motor manifestations. These seizures may present as tonic-clonic convulsions, during which the individual experiences muscle stiffening followed by rhythmic jerking movements. Absence seizures, characterized by brief lapses in consciousness, often go unnoticed due to their subtle nature, presenting as staring spells or brief episodes of unresponsiveness.
Additionally, individuals with epilepsy may experience prodromal symptoms, such as mood changes, sensory disturbances, or aura sensations, signaling the onset of a seizure. Postictal symptoms, occurring after a seizure, can include confusion, fatigue, headache, and muscle soreness, lasting minutes to hours. Beyond the physical manifestations, epilepsy can also impact cognitive function, behavior, and emotional well-being, contributing to psychosocial challenges and diminished quality of life. The varied presentation of epilepsy underscores the importance of comprehensive evaluation and individualized management strategies tailored to address the diverse needs of affected individuals.
By recognizing the nuanced symptoms and implementing timely interventions, healthcare providers can enhance seizure control, minimize complications, and improve overall outcomes for individuals living with epilepsy. (Nursing Paper Example on Epilepsy: Causes, Symptoms, Diagnosis, and Treatment [SOLVED])
![Nursing Paper Example on Epilepsy: Causes, Symptoms, Diagnosis, and Treatment [SOLVED]](https://www.carehospitals.com/ckfinder/userfiles/images/symptoms-of-epilepsy.png)
Etiology
The etiology of epilepsy is multifactorial, involving a complex interplay of genetic, developmental, structural, and environmental factors. Genetic predisposition plays a significant role, with numerous genes implicated in epilepsy susceptibility. Mutations in ion channel genes, such as SCN1A and KCNQ2, disrupt neuronal excitability and contribute to seizure initiation. Additionally, genetic syndromes like Dravet syndrome and Rett syndrome are characterized by epilepsy as a prominent feature. Developmental abnormalities in brain structure or connectivity also increase the risk of epilepsy. Prenatal insults such as maternal infections, intrauterine trauma, or exposure to teratogenic substances can disrupt normal brain development, predisposing individuals to epilepsy later in life.
Acquired brain injuries represent another common etiological factor, encompassing traumatic brain injuries, strokes, brain tumors, and infections. These insults disrupt neuronal networks and alter neurotransmitter balance, leading to hyperexcitability and seizure generation. Infections such as meningitis, encephalitis, and neurocysticercosis can directly affect brain function, triggering seizures as a pathological response.
Environmental factors further modulate epilepsy risk, with exposure to toxins, drugs, or metabolic disturbances influencing seizure susceptibility. Certain medications, such as antipsychotics and antidepressants, may lower seizure thresholds, exacerbating epilepsy in predisposed individuals. Metabolic imbalances, including electrolyte disturbances, hypoglycemia, and hypoxia, can precipitate seizures by disrupting neuronal homeostasis.
Understanding the diverse etiological factors contributing to epilepsy is crucial for accurate diagnosis and personalized treatment approaches. By identifying underlying causes and addressing predisposing factors, healthcare providers can optimize seizure control and improve outcomes for individuals living with epilepsy. Furthermore, ongoing research into the genetic and environmental determinants of epilepsy holds promise for developing novel therapeutic strategies and advancing precision medicine in epilepsy management. (Nursing Paper Example on Epilepsy: Causes, Symptoms, Diagnosis, and Treatment [SOLVED])
Pathophysiology
The pathophysiology of epilepsy encompasses a complex interplay of neuronal excitability, neurotransmitter dysregulation, and network abnormalities within the brain. Epilepsy arises from an imbalance between inhibitory and excitatory neurotransmission, disrupting the delicate equilibrium necessary for normal brain function.
Central to epilepsy’s pathophysiology is the concept of hyperexcitability, wherein neurons become excessively sensitive to excitatory stimuli. This heightened excitability may result from alterations in ion channel function, leading to abnormal neuronal firing patterns and synchronous activity across neuronal networks. Dysfunction in inhibitory neurotransmission, particularly involving gamma-aminobutyric acid (GABA), further exacerbates this imbalance, diminishing the brain’s ability to suppress aberrant neuronal firing.
Abnormalities in synaptic transmission and plasticity also contribute to epilepsy’s pathogenesis, altering the strength and stability of neuronal connections. Disruptions in synaptic plasticity mechanisms, such as long-term potentiation and long-term depression, may perpetuate epileptogenesis, facilitating the development and propagation of seizures.
Structural abnormalities within the brain, including cortical malformations, hippocampal sclerosis, and focal lesions, serve as focal points for seizure initiation and propagation. These structural anomalies disrupt normal neuronal architecture and connectivity, creating regions of hyperexcitability and epileptogenic foci.
Furthermore, neuroinflammatory processes, oxidative stress, and neurodegenerative changes contribute to epilepsy’s pathophysiology, exacerbating neuronal dysfunction and promoting seizure generation. Chronic epilepsy may lead to progressive neuronal damage and network reorganization, perpetuating the disorder and increasing the risk of treatment resistance.
Comprehending the intricate pathophysiological mechanisms underlying epilepsy is essential for developing targeted therapeutic interventions aimed at modulating neuronal excitability, restoring synaptic balance, and mitigating seizure activity. By unraveling the molecular and cellular determinants of epilepsy, researchers strive to identify novel therapeutic targets and advance precision medicine approaches for individuals living with this debilitating neurological condition. (Nursing Paper Example on Epilepsy: Causes, Symptoms, Diagnosis, and Treatment [SOLVED])
DSM-5 Diagnosis
The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), provides standardized criteria for diagnosing epilepsy and classifying seizure types. Diagnosis begins with a comprehensive medical history, neurological examination, and assessment of seizure semiology. Clinicians evaluate the frequency, duration, and characteristics of seizures, including motor, sensory, autonomic, and behavioral manifestations. Additionally, diagnostic tests such as electroencephalography (EEG), magnetic resonance imaging (MRI), and blood tests may be utilized to identify underlying causes and assess seizure localization.
DSM-5 criteria outline specific seizure types, including focal (partial) seizures and generalized seizures, each with distinctive features. Focal seizures originate in a localized area of the brain and may present with motor, sensory, autonomic, or psychic symptoms. Generalized seizures involve widespread neuronal activity and typically manifest as tonic-clonic convulsions, absence seizures, or myoclonic jerks.
Accurate diagnosis requires careful consideration of seizure semiology, electroclinical correlations, and ancillary investigations to differentiate epileptic seizures from other paroxysmal events. Differential diagnosis may include syncope, psychogenic nonepileptic seizures, movement disorders, and sleep-related phenomena.
Beyond seizure classification, DSM-5 criteria facilitate the diagnosis of epilepsy syndromes, which encompass a constellation of clinical features, electrographic patterns, and age of onset. Syndromic classification aids in prognostication, treatment selection, and genetic counseling, particularly in pediatric populations.
Overall, DSM-5 criteria serve as a valuable tool for standardizing epilepsy diagnosis, guiding clinical decision-making, and promoting consistency across healthcare settings. By adhering to these criteria and conducting thorough evaluations, clinicians can accurately identify epilepsy, tailor treatment regimens, and improve outcomes for individuals living with this neurological disorder. (Nursing Paper Example on Epilepsy: Causes, Symptoms, Diagnosis, and Treatment [SOLVED])
Treatment Regimens and Patient Education
Managing epilepsy requires a comprehensive approach aimed at controlling seizures, minimizing medication side effects, and enhancing quality of life. Treatment regimens typically involve a combination of pharmacological interventions, lifestyle modifications, and patient education.
Pharmacological Interventions: Antiepileptic drugs (AEDs) form the cornerstone of epilepsy treatment, with over twenty medications available for seizure management. The choice of AED depends on various factors, including seizure type, patient age, comorbidities, and medication tolerability. First-line AEDs such as carbamazepine, valproate, and levetiracetam are commonly prescribed to control seizure activity. However, treatment may require adjustments based on individual response and adverse effects. Periodic monitoring of drug levels and side effects is essential to optimize therapeutic outcomes and minimize medication-related complications.
Surgical Interventions: For individuals with medication-resistant epilepsy or focal seizure onset, surgical interventions may offer a viable treatment option. Surgical resection of epileptogenic brain tissue, such as the removal of hippocampal sclerosis or cortical dysplasia, can significantly reduce seizure frequency and improve long-term outcomes. Other surgical modalities, including vagus nerve stimulation (VNS) and deep brain stimulation (DBS), provide alternative approaches for seizure control in select cases.
Dietary Therapies: Dietary interventions, such as the ketogenic diet, offer non-pharmacological adjunctive treatment options for epilepsy management. The ketogenic diet, characterized by high fat, low carbohydrate intake, promotes ketosis and alters brain metabolism, reducing seizure frequency in some individuals, particularly those with medication-resistant epilepsy.
Patient Education: Empowering patients with knowledge about epilepsy, its management, and lifestyle modifications is essential for optimizing treatment outcomes and promoting self-management. Patient education initiatives should encompass information about seizure triggers, medication adherence, recognition of warning signs, and emergency protocols. Additionally, addressing psychosocial aspects, including stigma reduction, vocational support, and driving regulations, enhances patient well-being and social integration. Regular follow-up visits with healthcare providers facilitate ongoing education, medication adjustments, and seizure monitoring, fostering a collaborative approach to epilepsy management.
In conclusion, a holistic approach to epilepsy management integrates pharmacological, surgical, and lifestyle interventions, accompanied by comprehensive patient education. By addressing the diverse needs of individuals living with epilepsy and fostering empowerment through education and support, healthcare providers can improve seizure control, enhance quality of life, and promote holistic well-being. (Nursing Paper Example on Epilepsy: Causes, Symptoms, Diagnosis, and Treatment [SOLVED])

![Nursing Paper Example on Epilepsy: Causes, Symptoms, Diagnosis, and Treatment [SOLVED]](https://www.verywellhealth.com/thmb/-Vsr4a8cdIt0MGcTjC3KpkqoKzM=/1500x0/filters:no_upscale():max_bytes(150000):strip_icc()/IlloDot_Epilepsy-2f668bb5016a43ae95e4e15dce695346.png)