Nursing paper example on Asthma: Causes, Symptoms, Diagnosis, and Treatment
/in Assignment Help, Assignment Help Nursing, BLOG, Homework Help, Nursing Exam Help, Nursing Paper Help, Solved Nursing Essays /by Aimee GraceNursing paper example on Asthma: Causes, Symptoms, Diagnosis, and Treatment
Asthma, a chronic respiratory condition affecting millions worldwide, poses a significant health concern with its recurrent episodes of breathlessness, chest tightness, wheezing, and coughing, often exacerbated by environmental triggers. This paper aims to provide a comprehensive understanding of asthma, covering its causes, symptoms, etiology, pathophysiology, diagnostic criteria, treatment regimens, and patient education strategies. By delving into these aspects, this paper seeks to offer valuable insights for students and individuals seeking a deeper understanding of this prevalent ailment. Asthma’s impact extends beyond its physical manifestations, influencing various aspects of daily life and necessitating a multifaceted approach to management. Understanding the complexities of asthma is vital not only for healthcare professionals but also for patients and their caregivers in effectively navigating and mitigating the challenges posed by this chronic respiratory condition. (Nursing paper example on Asthma: Causes, Symptoms, Diagnosis, and Treatment)

Causes
Asthma’s origins lie in a complex interplay of genetic predispositions and environmental factors. Genetic susceptibility plays a significant role, with individuals having a family history of asthma or atopic conditions being at higher risk. Specific genes associated with asthma, such as those encoding proteins involved in immune regulation and airway inflammation, contribute to this predisposition.
Environmental triggers also play a crucial role in asthma development and exacerbation. Allergens, such as pollen, dust mites, pet dander, and mold, are common triggers, leading to allergic asthma. Non-allergic triggers include respiratory infections, exposure to tobacco smoke, air pollutants like particulate matter and nitrogen dioxide, and occupational exposures to chemicals or irritants.
Furthermore, early-life exposures and events can influence asthma development. Factors such as maternal smoking during pregnancy, low birth weight, premature birth, and early respiratory infections can increase the risk of developing asthma later in life. Additionally, lifestyle factors like obesity and sedentary behavior are associated with an increased likelihood of asthma.
Psychosocial factors, including stress and emotional disturbances, may also contribute to asthma onset and exacerbation. Stress-induced changes in immune function and airway inflammation can worsen asthma symptoms in susceptible individuals.
In summary, asthma is a multifactorial condition influenced by a combination of genetic predispositions, environmental exposures, early-life events, lifestyle factors, and psychosocial influences. Understanding these diverse causes is essential for developing effective prevention strategies and personalized treatment approaches tailored to address the specific triggers and risk factors affecting individuals with asthma. (Nursing paper example on Asthma: Causes, Symptoms, Diagnosis, and Treatment)
Signs and Symptoms
Asthma manifests with a variety of signs and symptoms, which can vary in severity and frequency among individuals. The hallmark symptoms of asthma include:
- Shortness of Breath: Asthma often presents with a sensation of breathlessness or difficulty breathing, particularly during physical activity or exposure to triggers.
- Chest Tightness: Many individuals with asthma experience tightness or discomfort in the chest, often described as a feeling of pressure or constriction.
- Wheezing: Wheezing is a common symptom characterized by a high-pitched whistling sound during breathing. It occurs due to the narrowing of the airways, leading to turbulent airflow.
- Coughing: Asthma-related coughing is typically dry and persistent, especially at night or early in the morning. It may worsen with exposure to allergens or irritants.
- Nighttime Symptoms: Asthma symptoms often worsen at night, disrupting sleep and causing nocturnal awakenings. Nighttime coughing and wheezing are particularly common.
- Exercise-Induced Symptoms: Physical exertion can trigger asthma symptoms in some individuals, leading to exercise-induced bronchoconstriction characterized by coughing, wheezing, and shortness of breath during or after exercise.
- Symptoms Triggered by Allergens or Irritants: Exposure to specific allergens or irritants, such as pollen, dust mites, pet dander, smoke, strong odors, or air pollution, can provoke asthma symptoms in susceptible individuals.
It’s important to note that asthma symptoms can fluctuate over time, with periods of symptom exacerbation (asthma attacks or exacerbations) alternating with periods of symptom improvement or remission. Additionally, the severity and frequency of symptoms can vary from person to person, and even within the same individual over time. Understanding the diverse presentation of asthma symptoms is crucial for accurate diagnosis and effective management of the condition. (Nursing paper example on Asthma: Causes, Symptoms, Diagnosis, and Treatment)
Etiology
The etiology of asthma is multifactorial, involving a complex interplay of genetic predispositions and environmental influences. Genetic factors play a significant role in asthma susceptibility, with numerous genes implicated in the regulation of immune responses, airway inflammation, and bronchial hyperreactivity. Variations in genes encoding cytokines, interleukins, and other immune-related proteins contribute to an individual’s risk of developing asthma.
Furthermore, environmental exposures play a crucial role in asthma development and exacerbation. Prenatal and early-life exposures, including maternal smoking during pregnancy, exposure to indoor and outdoor air pollutants, respiratory infections, and allergen exposure, significantly influence asthma risk. Maternal smoking during pregnancy, in particular, is associated with an increased risk of childhood asthma due to fetal exposure to tobacco smoke.
Early-life events, such as low birth weight, prematurity, and early respiratory infections, can also impact asthma development. These factors may alter lung development and immune function, increasing susceptibility to asthma later in life.
Moreover, lifestyle factors contribute to asthma etiology. Obesity is associated with an increased risk of asthma, possibly due to systemic inflammation and mechanical effects on the airways. Sedentary behavior and poor diet may also influence asthma risk through their effects on immune function and inflammation.
Psychosocial factors, including stress and emotional disturbances, have been implicated in asthma etiology. Stress-induced changes in immune function and airway inflammation can exacerbate asthma symptoms in susceptible individuals.
In summary, asthma etiology is multifaceted, involving a complex interplay of genetic predispositions, environmental exposures, early-life events, lifestyle factors, and psychosocial influences. Understanding these diverse etiological factors is essential for developing targeted prevention strategies and personalized treatment approaches aimed at mitigating asthma risk and improving outcomes for individuals affected by this chronic respiratory condition. (Nursing paper example on Asthma: Causes, Symptoms, Diagnosis, and Treatment)
Pathophysiology
Asthma pathophysiology involves a complex cascade of events within the respiratory system, characterized by chronic airway inflammation, airway hyperresponsiveness, and airflow limitation. This pathophysiological process is driven by a combination of genetic predispositions and environmental triggers.
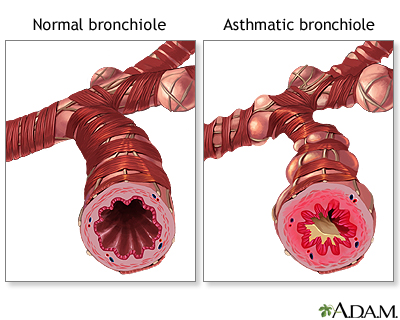
The initial phase of asthma pathophysiology involves the activation of inflammatory pathways in response to environmental triggers, such as allergens, respiratory infections, or air pollutants. This leads to the release of cytokines, chemokines, and other inflammatory mediators, resulting in the recruitment and activation of immune cells, including eosinophils, mast cells, and T lymphocytes, within the airways.
Chronic airway inflammation is a central feature of asthma pathophysiology, characterized by infiltration of inflammatory cells and increased production of pro-inflammatory cytokines and chemokines. This inflammatory milieu leads to structural changes in the airway walls, including epithelial damage, subepithelial fibrosis, and smooth muscle hypertrophy, collectively termed airway remodeling.
Airway hyperresponsiveness is another key aspect of asthma pathophysiology, referring to an exaggerated bronchoconstrictive response to various stimuli, such as allergens, exercise, or cold air. This heightened bronchial reactivity contributes to the characteristic symptoms of asthma, including wheezing, chest tightness, and dyspnea.
Airflow limitation occurs as a result of airway narrowing due to inflammation, smooth muscle contraction, mucus hypersecretion, and edema within the airway walls. This airflow limitation is reversible, either spontaneously or with treatment, distinguishing asthma from other obstructive respiratory conditions, such as chronic obstructive pulmonary disease (COPD).
In summary, asthma pathophysiology involves chronic airway inflammation, airway hyperresponsiveness, and airflow limitation, driven by a complex interplay of genetic predispositions and environmental triggers. Understanding these underlying pathophysiological mechanisms is crucial for developing targeted therapeutic strategies aimed at mitigating airway inflammation, reducing bronchial hyperreactivity, and improving long-term outcomes for individuals affected by asthma. (Nursing paper example on Asthma: Causes, Symptoms, Diagnosis, and Treatment)
DSM-5 Diagnosis
The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), does not provide specific diagnostic criteria for asthma. However, it recognizes the psychological impact of chronic respiratory conditions like asthma. Individuals with asthma may experience psychological distress, including anxiety or depression, due to various factors related to their condition.
Anxiety Disorders: Asthma-related anxiety can stem from the fear of experiencing asthma attacks, difficulty breathing, or the need for frequent medication use. Individuals with asthma may become hypervigilant about their respiratory symptoms, leading to heightened anxiety levels.
Depressive Disorders: The chronic nature of asthma and its impact on daily life activities can contribute to feelings of sadness, hopelessness, and loss of interest in previously enjoyable activities. Asthma-related limitations in physical activities, social interactions, and sleep disturbances may exacerbate depressive symptoms.
Adjustment Disorders: Asthma diagnosis or exacerbations can trigger adjustment difficulties characterized by emotional distress, impaired functioning, and maladaptive coping strategies. Individuals may struggle to adapt to the lifestyle changes necessitated by asthma management, leading to psychological distress.
Psychosocial Stressors: Environmental stressors, such as financial strain due to medical expenses, social stigma related to asthma, and difficulties in managing asthma in social or occupational settings, can exacerbate psychological distress in individuals with asthma.
The DSM-5 emphasizes the importance of considering the psychological impact of chronic medical conditions like asthma during clinical evaluations. Healthcare providers should assess for symptoms of anxiety, depression, and adjustment difficulties in individuals with asthma to facilitate appropriate interventions and support services. Psychoeducation, cognitive-behavioral therapy, and pharmacological treatments may be recommended to address psychological comorbidities and enhance overall well-being in individuals living with asthma. (Nursing paper example on Asthma: Causes, Symptoms, Diagnosis, and Treatment)
Treatment Regimens and Patient Education
Effective management of asthma involves a comprehensive approach that encompasses pharmacological interventions, non-pharmacological strategies, and patient education to optimize symptom control, prevent exacerbations, and improve quality of life.
Pharmacological Interventions: Pharmacotherapy forms the cornerstone of asthma management and aims to reduce airway inflammation, bronchial hyperresponsiveness, and symptoms. The main classes of asthma medications include:
- Inhaled Corticosteroids (ICS): ICS are the most effective anti-inflammatory medications for asthma and are recommended as first-line therapy for most patients. They reduce airway inflammation, thereby decreasing symptoms and the risk of exacerbations.
- Short-Acting Beta-Agonists (SABA): SABA, such as albuterol, provide rapid relief of asthma symptoms by relaxing the airway smooth muscles and relieving bronchoconstriction during acute exacerbations or as needed before exercise.
- Long-Acting Beta-Agonists (LABA): LABA, such as salmeterol and formoterol, are used as adjunct therapy in combination with ICS for long-term asthma control. They provide sustained bronchodilation and symptom improvement.
- Leukotriene Receptor Antagonists (LTRA): LTRA, such as montelukast, block the action of leukotrienes, which are inflammatory mediators involved in asthma. They are used as alternative or add-on therapy for patients unable to tolerate or adhere to ICS.
- Biologic Therapies: Biologic therapies, such as monoclonal antibodies targeting specific inflammatory pathways (e.g., anti-IgE, anti-IL-5), are reserved for severe, uncontrolled asthma characterized by eosinophilic or allergic inflammation.
Non-Pharmacological Strategies: Non-pharmacological interventions play a crucial role in asthma management and include:
- Allergen Avoidance: Identifying and avoiding specific allergens, such as dust mites, pollen, pet dander, and mold, can help reduce asthma symptoms and exacerbations.
- Smoking Cessation: Smoking cessation is essential for individuals with asthma, as tobacco smoke exposure worsens symptoms and reduces the efficacy of asthma medications.
- Regular Exercise: Regular physical activity, tailored to individual abilities, improves lung function, reduces asthma symptoms, and enhances overall well-being.
Patient Education: Patient education is fundamental in empowering individuals with asthma to manage their condition effectively. Key components of asthma education include:
- Trigger Identification: Educating patients about common asthma triggers and strategies to avoid or minimize exposure.
- Inhaler Technique: Ensuring patients understand the correct inhaler technique for optimal medication delivery and efficacy.
- Action Plans: Developing personalized asthma action plans that outline steps to take during symptom exacerbations or emergencies, including medication use and when to seek medical attention.
- Self-Management Strategies: Teaching patients self-monitoring techniques, such as peak flow monitoring, and empowering them to recognize and respond to changes in their asthma control.
- Medication Adherence: Emphasizing the importance of medication adherence and addressing any concerns or misconceptions patients may have about their asthma medications.
By implementing a multifaceted approach that combines pharmacological interventions, non-pharmacological strategies, and patient education, healthcare providers can optimize asthma management, improve patient outcomes, and enhance the overall quality of life for individuals living with asthma. (Nursing paper example on Asthma: Causes, Symptoms, Diagnosis, and Treatment)
Conclusion
Asthma is a complex chronic respiratory condition influenced by a multitude of factors, including genetic predispositions, environmental exposures, lifestyle choices, and psychosocial influences. Through this comprehensive exploration, we have elucidated the diverse causes, symptoms, etiology, pathophysiology, DSM-5 considerations, treatment regimens, and patient education strategies relevant to asthma management. Notably, we have highlighted the pivotal role of patient education in empowering individuals with asthma to effectively manage their condition through proper medication adherence, trigger identification, inhaler technique mastery, and self-management strategies. Moreover, the incorporation of both pharmacological interventions and non-pharmacological strategies, such as allergen avoidance and smoking cessation, underscores the importance of a holistic approach in optimizing asthma control and improving patient outcomes. By understanding and addressing the multifaceted nature of asthma, healthcare providers can enhance their ability to provide personalized care and support to individuals living with this prevalent respiratory ailment, ultimately improving their quality of life. (Nursing paper example on Asthma: Causes, Symptoms, Diagnosis, and Treatment)






 Causes
Causes:max_bytes(150000):strip_icc()/VWH_Illustration_Allergen-Types-and-Triggers_Illustrator_Sydney-Saporito_Final-00bb7f7393d6436e9dc347e85a0ec0b3.jpg)

:max_bytes(150000):strip_icc()/hiv-aids-symptoms-4014373-final-ct-003ab16aa2f64faa9209cf4e6a71a555.png)