Major Depressive Disorder Focused SOAP Note
Major Depressive Disorder Focused SOAP Note
Major Depressive Disorder Focused SOAP Note
Comprehensive Focused SOAP Note Psychiatric Evaluation on Major Depressive Disorder
Patient Initials: K.W.
Gender: Female
Age: 35 years
SUBJECTIVE:
CC: “I feel down, and I fear for my job because I have lagged in most tasks for the past three months.”
HPI: K.W. is a 35-year-old female patient presenting at the clinic with complaints of feeling down most of the time. She reports that for the last three months, she has submitted most of her work assignments late and she now fears for her job, with two warnings already. K.W. reports feeling hopeless about her future. She lost her younger sister to illness one year ago, and she has struggled to recover from it. After losing her parents five years ago, she took the sole responsibility of caring for her younger sister. However, the past year her sister fell ill with pneumonia and succumbed after two months of illness. This death was a blow, making her feel she failed her parents and her sister because she was not around a lot due to job responsibilities and having no one else to take care of her sister, besides her husband, who was also out most of the time for work. The patient claims she also fears for her marriage, and she has not stopped worrying that her life is not going well for the last three months. Her feeling down and anxiety cannot let her concentrate on taking care of her family and doing her job assignments properly. K.W. has lost social contact with her friends and workmates and claims her husband is complaining of lost intimacy. K.W. struggles to fall or stay asleep, sleeping for about 2-4 hours every night. Her appetite has reduced, and she eats canned or ordered food most of the time, which her husband does not appreciate. K.W. has taken alprazolam 1mg in the past month to control her anxiety about her life, marriage, job, and future. She has also taken cannabis several times, claiming it makes her feel relaxed. Additionally, the patient claims to using alcohol, but secretly because she does not want her husband and friends to know. K.W. comes in seeking help to take control of her life again. (Comprehensive Focused SOAP Note Psychiatric Evaluation on Major Depressive Disorder )
Social History: K.W. has lived in Texas most of her life, but moved to Minnesota seven years ago for work duties. She met her husband five years ago after her parent’s death and they got married three years ago. She currently lives with her husband.
Education and Occupation History: K.W. has a Supply Chain Management Degree from Texas State University. She also completed her MBA at the same university. K.W. currently works as a procurement director at her current workplace.
Substance Current Use and History: The client claims to have used marijuana in the past month because it makes her feel relaxed. She is also secretly taking alcohol to control her stress level.
Legal History: The client denies any legal history.
Family Psychiatric/Substance Use History: K.W. denies a family psychiatric history. Her father and mother used alcohol occasionally, especially on weekends.
Past Psychiatric History:
Hospitalization: K.W. denies hospitalization from a mental health issue.
Medication trials: K.W. denies a history of medication trials
Psychotherapy or Previous Psychiatric Diagnosis: K.W. denies previous psychiatric evaluation
Medical History: K.W. was hospitalized in 2012 after an allergic reaction to shellfish.
- Current Medications:W. reports taking alprazolam 1mg twice daily.
- Allergies:W. is allergic to seafood.
- Reproductive Hx:Sexually active. K.W. reports not using any birth control because they have been trying to have their first baby. Her last menses was one and a half months ago.
ROS:
General: K.W. states her appetite has reduced and she feels weak when she wakes up early in the morning. Her frequent feelings of fatigue have affected her ability to do house chores for the past three months. She denies fever.
HEENT: Eyes: K.W. denies visual loss, blurred vision, double vision, or yellow sclerae. Ears, Nose, Throat: No hearing loss, sneezing, congestion, runny nose, or sore throat.
Skin: No rash or itching.
Cardiovascular: Denies chest pain, chest pressure, or chest discomfort. No palpitations or edema.
Respiratory: Denies wheezes, shortness of breath, consistent coughs, and breathing difficulties while resting. (Comprehensive Focused SOAP Note Psychiatric Evaluation on Major Depressive Disorder )
Gastrointestinal: K.W. reports reduced appetite, and diet changes as she mostly eats canned or ordered food. She feels nauseated after most meals. K.W. denies vomiting and diarrhea. No abdominal pain or blood. The patient reports experiencing constipation.
Genitourinary: Denies burning on urination, urgency, hesitancy, odor, odd color
Neurological: K.W. states that she experiences frequent headaches and dizziness, especially after waking up. She denies syncope, paralysis, ataxia, numbness, or tingling in the extremities. No change in bowel or bladder control. K.W. reports concentration and attention difficulties at work.
Musculoskeletal: K.W. states she experiences occasional muscle pain and weakness. She denies back pain and muscle or joint stiffness.
Hematologic: Denies anemia, bleeding, or bruising.
Lymphatics: Denies enlarged nodes. No history of splenectomy.
Endocrinologic: K.W. reports sweating when she feels anxious about her job, marriage, and life. She denies cold or heat intolerance. No polyuria or polydipsia.
OBJECTIVE: (Comprehensive Focused SOAP Note Psychiatric Evaluation on Major Depressive Disorder )
Vital signs: Stable
Temp: 97.5F
B.P.: 125/70
P: 87
R.R.: 17
O2: Room air
Pain: 2/10
Ht: 5’5 feet
Wt: 140 lbs
BMI: 23.3
BMI Range: Healthy weight
LABS:
Lab findings WNL
Tox screen: Positive
Alcohol: Positive
Physical Exam:
General appearance: K.W. appears moody, disturbed, and stressed, breaking down in two occasions. She seems anxious about being at the clinic. However, K.W. appears well-fed and nourished and is well-groomed and dressed for the time, place, and occasion. K.W. was polite and engaged the interviewer appropriately. The patient is well-groomed. The patient addressed the interviewer in a polite and regular manner. The patient struggled to maintain concentration and attention throughout the interview. (Comprehensive Focused SOAP Note Psychiatric Evaluation on Major Depressive Disorder )
HEENT: Normocephalic and atraumatic. Sclera anicteric, No conjunctival erythema, PERRLA, oropharynx red, moist mucous membranes.
Neck: Supple. No JVD. Trachea midline. No pain, swelling, or palpable nodules.
Heart/Peripheral Vascular: Regular rate and rhythm noted. No murmurs. No palpitation. No peripheral edema to palpation bilaterally.
Cardiovascular: Regular heartbeat and rhythm. K.W.’s heart rate is within normal range, and capillaries refill within two and a half seconds.
Musculoskeletal: K.W. indicated a regular range of motion and muscle mass for age. No signs of swelling or joint deformities. Muscle and back pain rated 2/10.
Respiratory: K.W. indicated regular and easy respirations without wheezes.
Neurological: K.W.’s balance is stable, gait is normal, posture is erect, the tone is good, and speech is clear. K.W. has frequent headaches and dizziness.
Psychiatric: K.W. appeared moody, disturbed, stressed, and anxious. She has insomnia and indicated impaired concentration and attention.
Neuropsychological testing: K.W. indicates impaired social, emotional, and occupational functioning. (Comprehensive Focused SOAP Note Psychiatric Evaluation on Major Depressive Disorder )
Behavior/motor activity: K.W.’s behavior and engagement were appropriate and constant during the interview.
Gait/station: Stable.
Mood: Depressed and anxious mood.
Affect: Disturbed.
Thought process/associations: relatively linear and impaired.
Thought content: Thought content is inconsistent.
Attitude: K.W. was polite and engaged appropriately with the interviewer.
Orientation: K.W. was oriented to self, place, situation, and time.
Attention/concentration: K.W. indicated impaired concentration and attention.
Insight: Good
Judgment: Good.
Remote memory: Good
Short-term memory: Good
Intellectual /cognitive function: Good
Language: Clear speech and normal tone
Fund of knowledge: Good.
Suicidal ideation: Positive with no active plans.
Homicide ideation: Negative.
ASSESSMENT:
Mental Status Examination:
The 35-year-old female patient complains of feeling down and worried most of the time. She feels hopeless about her future life and fears for her job and marriage. During the assessment, K.W. was oriented to self, place, situation, and time. She expressed a depressed and anxious mood. Her thought process was relatively linear but impaired, with an inconsistent thought content. However, K.W. was polite and engaged appropriately with the interviewer. The patient indicated impaired concentration and attention. Her insight, judgment, and memory were good. Her speech was clear and her tone was normal. She indicated a good fund of knowledge. K.W. reported having suicidal ideation but is negative of any active plans. She denied any homicidal ideation. (Comprehensive Focused SOAP Note Psychiatric Evaluation on Major Depressive Disorder )
Diagnostic Impression:
- 9 Major Depressive Disorder
- 1 Generalized Anxiety Disorder
- 81 Prolonged Grief Disorder
Differential Diagnosis:
- 9 Major Depressive Disorder
K.W. indicates signs of depression. K.W. reports that she feels down most of the time, especially in the last three months. She cannot complete her job assignments or house chores due to her feeling down and stressed. She fears she will get fired and break her marriage because the husband shows concerns over her late behavior, including not cooking home meals, loss of intimacy, and anti-social patterns. The patient reports feeling hopeless about her future. She has sleeping difficulties, sleeping 2-4 hours daily. The patient also reports reduced appetite and loss of concentration and attention. Per the DMS-5 criteria, for MDD to be confirmed, the patient must present with at least five of the following symptoms: sleeping difficulties, concentration, and attention difficulties, feelings of helplessness and inadequacy, feelings of tiredness and erratic energy, appetite and weight changes, suicidality, depressed mood, and psychomotor issues (Chand et al., 2021). The patient presents with at least five of these symptoms, confirming MDD. (Comprehensive Focused SOAP Note Psychiatric Evaluation on Major Depressive Disorder )
- 1 Generalized Anxiety Disorder
K.W. presents with signs of generalized anxiety disorder. The patient indicates an anxious mood. She is worried a lot and almost all the time about her future, her job, her marriage, and her life. The patient fears she will be fired, having received two warnings in the last three months. K.W. also fears she will break her marriage because she has demonstrated anti-social behavior, does not engage in home cooking, and has reduced intimacy, which her husband is not happy about. For GAD to be confirmed per the DMS-5 criteria, the patient has to present with intense anxiety and worry happening more days than not for a minimum of 6 months about different events or activities, difficulty controlling the worry, at least three symptoms of restlessness, fatigue, struggling to concentrate and blankness, irritability, muscle tension, sleep disturbance due to the anxiety and worry, the disturbance is not better explained by another mental illness, the anxiety, worry, and physical symptoms lead to severe clinical distress or impairment in occupational, social, and other functional areas, and the disturbance is not due to physiological effects of substance use (Munir & Takov, 2022). K.W. presents with most of the indicated symptoms, but MDD better explains the presented symptoms and she does not fit all criteria, refuting the diagnosis. Further assessment is needed during the follow-up. (Comprehensive Focused SOAP Note Psychiatric Evaluation on Major Depressive Disorder )
- 81 Prolonged Grief Disorder (PGD)
The patient indicates signs of PGD. K.W. appears not to have recovered from grieving the loss of her younger sister to illness a year ago. The patient reports that her death was devastating because she took the sole responsibility of caring for her after their parents died five years ago. However, she was not around mostly due to work and her sister developed pneumonia, which was implicated in her death. The patient’s depressed mood and anxiety are linked to this event, and K.W. appears not to have recovered fully from it. For prolonged grief disorder to be confirmed per the DMS-5 criteria, the patient must have lost someone at least 12 months earlier (Criterion A), experience severe yearning or preoccupation (Criterion B), in addition to at least 3 symptoms of identity disruptions, avoidance, disbelief, emotional pain, struggles to move on, numbness, a sense of meaninglessness in life, and loneliness (Criterion C), for about a month, leading to distress or disability (Criterion D), exceed cultural and contextual norms (Criterion E), and the symptoms are not better justified by another mental disorder (Criterion F) (Boelen et al., 2020). K.W. presents with most of the indicated symptoms but does not fit all criteria, refuting PGD. However, the seriousness of the case requires more assessment to confirm the diagnosis of PGD. (Comprehensive Focused SOAP Note Psychiatric Evaluation on Major Depressive Disorder )
Reflection:
The interview went well and the patient provided pertinent information to guide diagnosis and treatment plan development. However, further assessment is warranted as the patient indicated being positive for most symptoms of generalized anxiety disorder and prolonged grief disorder, although these diagnoses were not confirmed in this encounter per the DMS-5 criteria. In another encounter with the patient, I would adopt GAD-7 and PGD scales to assess the two diagnoses further. I would also inquire from the husband about the experience at home and how the patient has coped with her situation. It would also be helpful to gather information from her workplace to establish robust data to guide a more specific diagnosis. (Comprehensive Focused SOAP Note Psychiatric Evaluation on Major Depressive Disorder )
Engaging patients presenting with signs of depression, anxiety, a grief can be ethically challenging because the practitioner must maintain respect for persons, especially when the patient expresses disinterest, irritability, and is uncooperative. The practitioner must also promote patient autonomy, truthfulness, non-disclosure, beneficence, and nonmaleficence. For instance, when prescribing for pain management and other symptoms, the practitioner must consider harmful side effects. Treatment refusal is common, and the provider must communicate effectively to ensure the patient makes informed decisions. The practitioner should recommend strategies to promote the patient’s health, including establishing a conducive and supporting home environment, recommending social skills training, encouraging activities like exercise, yoga, and meditation, and promoting home-cooked meals with the husband (Binghamton University, 2021). The patient wants to feel her emotions and feelings recognized, acknowledged, and supported to help address them. (Comprehensive Focused SOAP Note Psychiatric Evaluation on Major Depressive Disorder )
Case Formulation and Treatment Plan:
The patient would benefit from a combination of pharmacological and psychotherapy interventions.
Safety Risk/Plan:
K.W. is suicidal with no active plans. The patient is not homicidal. Psychotherapy will help address the suicidality and hospitalization is not necessary now.
Pharmacological Interventions:
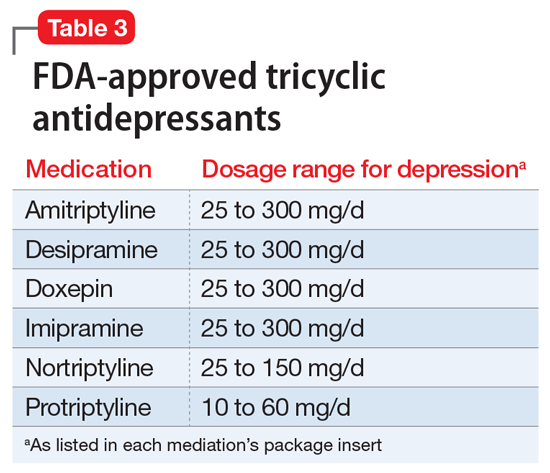
K.W. can benefit from antidepressants that will help reduce and manage depressive symptoms. The patient will be prescribed selected serotonin reuptake inhibitors like fluoxetine and citalopram as first-line treatment of depressive symptoms (Chand et al., 2021). The patient will continue with alprazolam 1 mg twice daily to address her anxiety (George & Tripp, 2023). Combining antidepressants, antipsychotics, and mood stabilizers will be more effective in achieving optimal outcomes like improving her mood and energy. The patient will also be prescribed Rozerem 8 mg, taken 30 minutes before bed, to help improve the quality of her sleep. (Comprehensive Focused SOAP Note Psychiatric Evaluation on Major Depressive Disorder )
Psychotherapy:
The patient needs psychotherapy to help improve depressive, anxiety, and grieving symptoms. K.W. will receive sessions of psychotherapy for two hours, three days a week for the next one month. Family-based therapy is recommended to help assess, analyze, and reorganize essential elements in her family environment, like her relationship and intimacy with her husband, and create a supporting home environment. Cognitive behavioral therapy CBT is recommended to improve her thinking patterns and behavior by addressing the emotions and feelings of being trapped in a cycle of feelings of hopelessness, stress, down, anxiety, and worry (Chand et al., 2021). CBT will help improve K.W.’s awareness of her thoughts, feelings, emotions, and beliefs, and modify those to improve her overall mood. (Comprehensive Focused SOAP Note Psychiatric Evaluation on Major Depressive Disorder )
Education:
- Educate the patient about medication side effects, when to report side effects, and the importance of medication and psychotherapy adherence.
- Guide the patient through lifestyle changes like healthy eating and physical activity.
- Recommend participating in support groups and group therapy to address the anti-social behavior.
Consultation/follow-up: Follow-up is in two weeks for further assessment. (Comprehensive Focused SOAP Note Psychiatric Evaluation on Major Depressive Disorder )


