Nursing Paper Example on a Comprehensive Overview of Cerebral Palsy: Etiology, Diagnosis, Treatment, and Patient Empowerment
Nursing Paper Example on a Comprehensive Overview of Cerebral Palsy: Etiology, Diagnosis, Treatment, and Patient Empowerment
Causes
Cerebral palsy (CP) stems from a multitude of factors, encompassing prenatal, perinatal, and postnatal origins. Prenatally, maternal infections, such as rubella or cytomegalovirus, can significantly increase the risk of CP. Genetic mutations and chromosomal abnormalities, though less frequent, are also implicated. Intrauterine growth restriction (IUGR) and maternal health issues like thyroid disorders or hypertension during pregnancy contribute to the prenatal landscape of CP.
Perinatal factors play a pivotal role in CP development. Birth asphyxia, resulting from oxygen deprivation during labor or delivery, remains a critical risk factor. Prematurity, defined as birth before 37 weeks of gestation, exposes infants to vulnerabilities in brain development, increasing CP risk. Low birth weight, often associated with prematurity, is another determinant, as it can lead to underdeveloped brain structures and heightened susceptibility to injury.
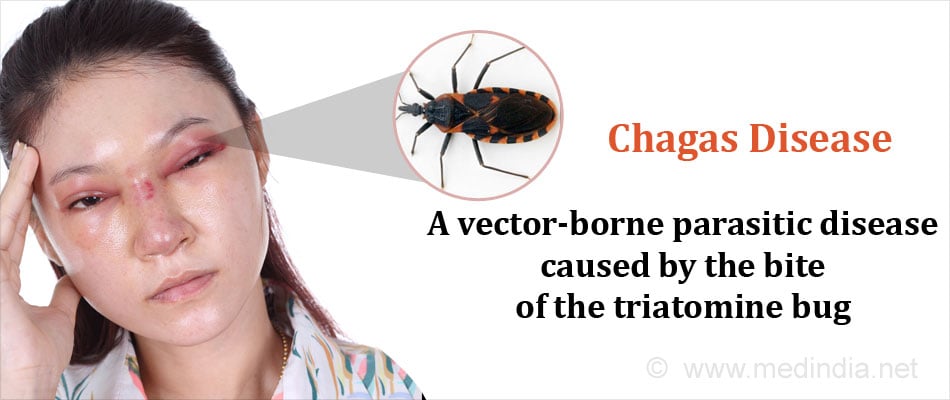
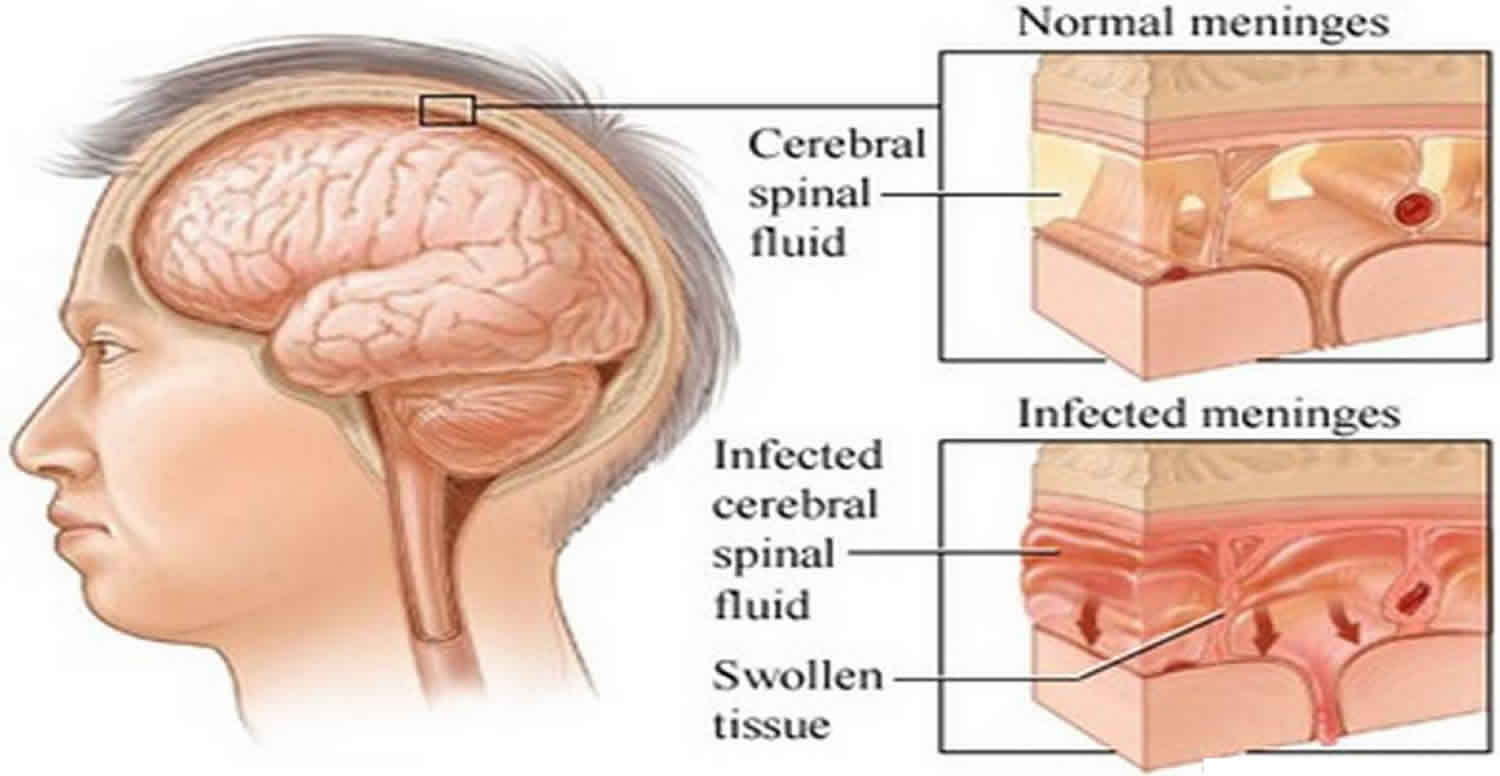
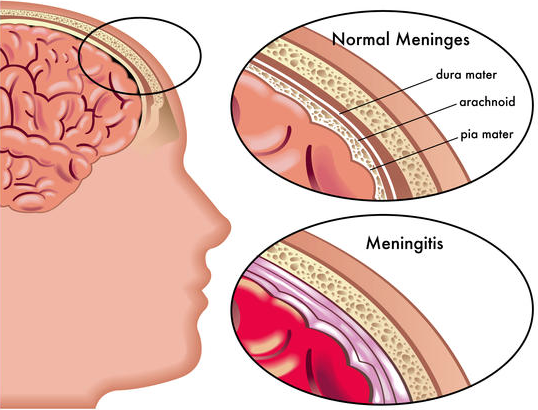
Postnatally, brain injuries during infancy or early childhood significantly contribute to CP. Infections like meningitis or encephalitis can cause inflammation and damage to brain tissue, impacting motor function. Traumatic brain injuries resulting from accidents or non-accidental trauma, such as shaken baby syndrome, are also potential triggers for CP. Additionally, strokes occurring in infancy or childhood can disrupt blood flow to the brain, leading to cerebral palsy.
While the exact mechanisms underlying CP causation remain intricate and multifaceted, understanding these diverse factors is crucial for prevention, early detection, and intervention strategies. Initiatives aimed at minimizing risk factors, promoting maternal health, and ensuring access to quality prenatal and perinatal care can play a pivotal role in reducing the incidence of cerebral palsy and improving outcomes for affected individuals. (Nursing Paper Example on a Comprehensive Overview of Cerebral Palsy: Etiology, Diagnosis, Treatment, and Patient Empowerment)
Signs and Symptoms
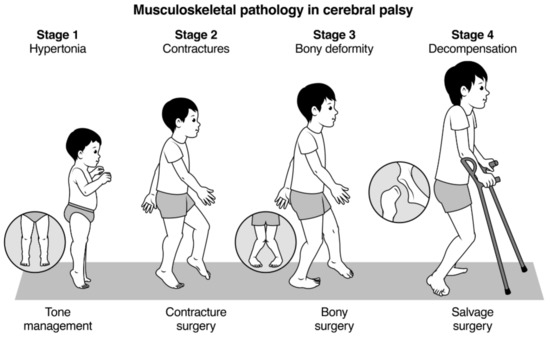
Cerebral palsy (CP) manifests in a spectrum of signs and symptoms, reflecting its heterogeneous nature and diverse impact on motor function and development. Impaired movement and coordination are hallmark features of CP, characterized by difficulties in controlling muscles and executing precise movements. Muscle stiffness or spasticity, often accompanied by involuntary muscle contractions, contributes to the overall motor impairment seen in CP.
Abnormal reflexes, such as exaggerated or absent reflex responses, are commonly observed in individuals with CP. These reflex abnormalities further hinder movement coordination and contribute to difficulties in achieving and maintaining posture and balance. As a result, individuals with CP may exhibit abnormal gait patterns, including toe-walking, scissoring of the legs, or asymmetrical movements.
In addition to motor impairments, CP frequently presents with associated conditions that impact overall functioning and quality of life. Intellectual disabilities, ranging from mild to severe, affect cognitive abilities and learning potential in varying degrees. Seizures, occurring in up to half of individuals with CP, pose additional challenges and require careful management to minimize their impact on daily activities.
Sensory impairments, including visual and auditory deficits, are also prevalent among individuals with CP, further complicating their ability to interact with their environment. Behavioral challenges, such as impulsivity, hyperactivity, or difficulties with social interactions, may arise due to the underlying neurological differences associated with CP.
The combination of motor impairments, associated conditions, and sensory and behavioral challenges underscores the complex nature of cerebral palsy and its wide-ranging impact on individuals’ lives. Early recognition of signs and symptoms, coupled with comprehensive multidisciplinary assessments, is crucial for timely intervention and support to optimize outcomes for individuals living with CP. (Nursing Paper Example on a Comprehensive Overview of Cerebral Palsy: Etiology, Diagnosis, Treatment, and Patient Empowerment)
Etiology
The etiology of cerebral palsy (CP) is multifactorial and often involves complex interactions between genetic, environmental, and developmental factors. Prenatal influences play a significant role in shaping CP risk, with maternal health and prenatal exposures impacting fetal brain development. Maternal infections, such as rubella or cytomegalovirus, can lead to neuroinflammation and disrupt normal brain development, increasing the likelihood of CP.
Genetic factors contribute to CP susceptibility, although their role is not always straightforward. Genetic mutations and chromosomal abnormalities may predispose individuals to CP, affecting neurodevelopmental processes critical for motor function and coordination. Additionally, variations in genes related to neuronal growth, synapse formation, and neurotransmitter regulation may influence CP risk.
Perinatal factors exert a substantial influence on CP etiology, with events occurring around the time of birth playing a pivotal role. Birth asphyxia, resulting from oxygen deprivation during labor or delivery, can lead to brain hypoxia and subsequent injury, contributing to CP development. Premature birth, defined as birth before 37 weeks of gestation, exposes infants to vulnerabilities in brain development, increasing CP risk.
Postnatal factors, including brain injuries and infections during infancy or early childhood, also contribute to CP etiology. Traumatic brain injuries, such as those resulting from accidents or non-accidental trauma, can cause structural damage to the brain, disrupting motor pathways and leading to CP. Infections like meningitis or encephalitis can result in neuroinflammation and neuronal damage, further exacerbating CP risk.
The interplay of these diverse etiological factors highlights the complexity of CP development and underscores the importance of a comprehensive approach to understanding its origins. Continued research into the genetic, environmental, and developmental determinants of CP is essential for elucidating its etiology and informing strategies for prevention, early intervention, and improved outcomes for affected individuals. (Nursing Paper Example on a Comprehensive Overview of Cerebral Palsy: Etiology, Diagnosis, Treatment, and Patient Empowerment)
Pathophysiology
The pathophysiology of cerebral palsy (CP) involves complex disruptions in brain development and function, affecting motor control, muscle tone, and coordination. While the precise mechanisms underlying CP pathogenesis vary among individuals, several key processes contribute to its manifestations.
Abnormalities in brain development, particularly during the prenatal and perinatal periods, play a central role in CP pathophysiology. Disturbances in neuronal migration, which occur during early brain development, can lead to structural abnormalities and impaired connectivity within the brain. Disruptions in white matter development, characterized by abnormalities in myelination and axonal connectivity, further impair the transmission of neural signals involved in motor control.
Neuroinflammation and oxidative stress are also implicated in CP pathophysiology, contributing to neuronal damage and functional impairments. Inflammatory responses triggered by prenatal infections, perinatal hypoxia-ischemia, or postnatal insults lead to the release of pro-inflammatory cytokines and reactive oxygen species, exacerbating neuronal injury and impairing neurodevelopmental processes.
Alterations in neurotransmitter systems, including imbalances in excitatory and inhibitory neurotransmission, contribute to motor dysfunction and spasticity in CP. Imbalances in neurotransmitters such as glutamate and gamma-aminobutyric acid (GABA) disrupt the delicate balance of neuronal signaling, leading to increased muscle tone and impaired motor control.
Structural abnormalities within specific brain regions, such as the basal ganglia and cerebellum, are commonly observed in individuals with CP and contribute to motor impairments. Dysfunction within these regions disrupts the coordination of voluntary movements and postural control, further exacerbating motor difficulties.
The cumulative effects of these pathophysiological processes result in the diverse manifestations of CP, including impaired movement, muscle stiffness, abnormal reflexes, and associated comorbidities. Understanding the underlying pathophysiology of CP is essential for developing targeted interventions aimed at mitigating its impact and improving outcomes for affected individuals. (Nursing Paper Example on a Comprehensive Overview of Cerebral Palsy: Etiology, Diagnosis, Treatment, and Patient Empowerment)
DSM-5 Diagnosis
The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), provides criteria for diagnosing cerebral palsy (CP) based on motor impairments and evidence of neurological abnormalities. The DSM-5 criteria emphasize the importance of a comprehensive medical evaluation to accurately diagnose CP and differentiate it from other motor disorders.
The primary criterion for CP diagnosis involves the presence of motor impairments that significantly interfere with movement and posture. These motor impairments typically manifest as abnormalities in muscle tone, coordination, and control, affecting both gross and fine motor skills. Examples include spasticity, muscle stiffness, involuntary movements, and difficulties with balance and coordination.
The onset of motor impairments is another key criterion for CP diagnosis according to DSM-5 guidelines. Motor symptoms must be evident before the age of 2 to meet the diagnostic criteria for CP. Early recognition of motor abnormalities and developmental delays is crucial for timely diagnosis and intervention.
In addition to motor impairments, the DSM-5 criteria for CP diagnosis require evidence of neurological abnormalities consistent with the disorder. Neurological assessments, including imaging studies such as magnetic resonance imaging (MRI) or computed tomography (CT) scans, may reveal structural brain abnormalities or signs of perinatal brain injury consistent with CP.
The DSM-5 also emphasizes the importance of ruling out other conditions that may mimic CP or coexist with it. Differential diagnosis may involve evaluating for other neurological disorders, musculoskeletal conditions, or developmental disabilities that share similar clinical features with CP.
A comprehensive evaluation incorporating clinical assessment, neurological examinations, developmental assessments, and imaging studies is essential for accurate CP diagnosis according to DSM-5 criteria. Timely and accurate diagnosis facilitates appropriate interventions, including early intervention services, rehabilitation therapies, and support services, to optimize outcomes for individuals living with CP. (Nursing Paper Example on a Comprehensive Overview of Cerebral Palsy: Etiology, Diagnosis, Treatment, and Patient Empowerment)
Treatment Regimens and Patient Education
The management of cerebral palsy (CP) involves a multidisciplinary approach aimed at addressing the diverse needs of individuals with CP and optimizing their overall function and quality of life. Treatment regimens for CP are tailored to the specific needs and challenges of each individual and may encompass various therapeutic interventions, support services, and patient education initiatives.
Therapeutic Interventions:
Physical therapy plays a central role in CP management, focusing on improving mobility, strength, flexibility, and motor function. Therapeutic exercises, stretching routines, and gait training are integral components of physical therapy programs tailored to the unique needs of individuals with CP.
Occupational therapy aims to enhance independence and participation in daily activities by addressing fine motor skills, sensory integration, and adaptive strategies. Occupational therapists work with individuals with CP to develop skills necessary for self-care, school, work, and recreational activities.
Speech therapy targets communication and swallowing difficulties commonly associated with CP. Speech-language pathologists assess and address speech articulation, language development, and oral motor function to improve communication and feeding skills.
Medications may be prescribed to manage spasticity, muscle stiffness, seizures, and associated comorbidities in individuals with CP. Common medications include muscle relaxants, antispasmodics, antiepileptic drugs, and medications to alleviate pain or discomfort.
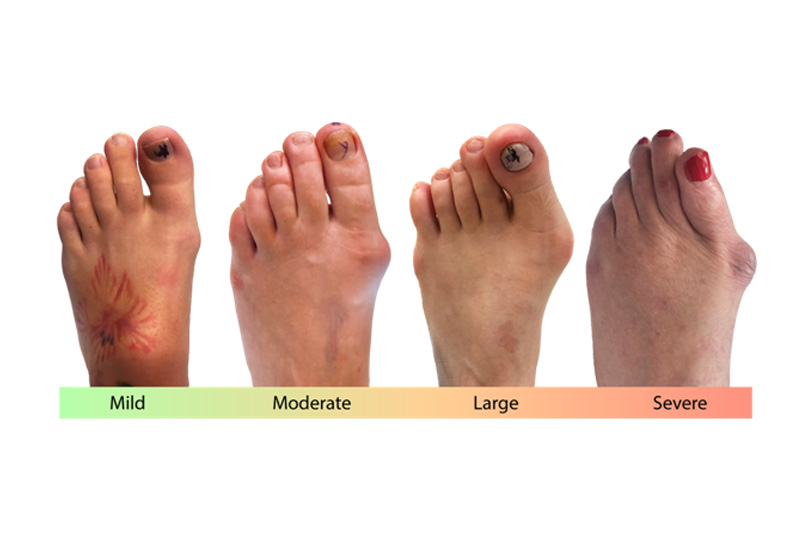
Orthotic devices, such as braces, splints, or orthopedic footwear, may be recommended to improve posture, stability, and mobility in individuals with CP. Orthotics help support weakened muscles, correct alignment issues, and facilitate optimal movement patterns.
Patient Education:
Patient education is an essential component of CP management, empowering individuals with CP and their families to actively participate in treatment plans, access support services, and make informed decisions about their care. Education initiatives for individuals with CP may include:
- Providing information about the nature of CP, including its causes, symptoms, and prognosis.
- Educating individuals and families about available treatment options, including therapeutic interventions, medications, and surgical procedures.
- Offering guidance on accessing support services, such as early intervention programs, special education services, and community resources.
- Providing strategies for managing daily challenges associated with CP, including mobility limitations, communication difficulties, and behavioral issues.
- Promoting self-advocacy skills and encouraging individuals with CP to express their needs, preferences, and goals in healthcare settings and beyond.
By incorporating therapeutic interventions and patient education initiatives into comprehensive treatment regimens, healthcare professionals can effectively support individuals with CP in achieving their maximum potential and enhancing their overall well-being. (Nursing Paper Example on a Comprehensive Overview of Cerebral Palsy: Etiology, Diagnosis, Treatment, and Patient Empowerment)




 Chlamydia infection can manifest with a wide range of signs and symptoms, although many individuals infected with Chlamydia trachomatis remain asymptomatic, especially in the early stages of infection. When symptoms do occur, they typically appear within 1 to 3 weeks after exposure to the bacterium.
Chlamydia infection can manifest with a wide range of signs and symptoms, although many individuals infected with Chlamydia trachomatis remain asymptomatic, especially in the early stages of infection. When symptoms do occur, they typically appear within 1 to 3 weeks after exposure to the bacterium.





 Causes
Causes