Nursing Paper Example on Gastrointestinal Disease: Gastroesophageal Reflux Disease (GORD)
Nursing Paper Example on Gastrointestinal Disease: Gastroesophageal Reflux Disease (GORD)
Introduction
Gastroesophageal Reflux Disease (GORD) is a prevalent gastrointestinal ailment affecting millions worldwide. Characterized by the backward flow of stomach acid into the esophagus, GORD poses significant discomfort and potential health risks if left untreated. The lower esophageal sphincter’s weakened state allows gastric contents to regurgitate, causing symptoms like heartburn, chest pain, and regurgitation. While the exact prevalence varies across demographics, GORD is commonly associated with factors such as obesity, smoking, and certain medications. Understanding the underlying mechanisms of GORD is crucial for effective management and prevention of complications. This essay explores the causes, symptoms, etiology, pathophysiology, diagnosis, treatment regimens, and patient education strategies related to GORD, shedding light on its impact on individuals’ daily lives and the importance of comprehensive management approaches. (Nursing Paper Example on Gastrointestinal Disease: Gastroesophageal Reflux Disease (GORD))
Causes
Gastroesophageal Reflux Disease (GORD) stems from various factors, primarily centered around the malfunctioning of the lower esophageal sphincter (LES), a muscular ring separating the esophagus from the stomach. This weakening or relaxation of the LES allows stomach acid and partially digested food to flow backward into the esophagus, leading to the characteristic symptoms of GORD.
One of the significant causes of LES dysfunction is obesity. Excess weight puts pressure on the abdomen, which can force stomach contents upward into the esophagus, particularly when lying down or bending over. Additionally, adipose tissue produces hormones and substances that may contribute to LES relaxation, exacerbating reflux symptoms in obese individuals.
Smoking is another prominent risk factor for GORD. The chemicals in cigarette smoke can weaken the LES and impair its ability to prevent acid reflux. Moreover, smoking reduces saliva production, which normally helps neutralize stomach acid in the esophagus. Consequently, smokers are more prone to experiencing severe and prolonged reflux symptoms.
Certain medications are known to exacerbate GORD symptoms or weaken the LES. These include nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen and aspirin, which can irritate the esophageal lining and increase acid production, aggravating reflux symptoms. Other medications, such as calcium channel blockers used to treat hypertension and some sedatives, may relax the LES, facilitating acid reflux.
Dietary factors play a crucial role in triggering GORD symptoms. Spicy, acidic, and fatty foods can irritate the esophagus and stimulate acid production, exacerbating reflux. Citrus fruits, tomatoes, chocolate, caffeine, and alcohol are common culprits known to worsen symptoms in susceptible individuals. Moreover, large meals and lying down shortly after eating can increase intra-abdominal pressure, promoting acid reflux.
Pregnancy is also associated with an increased risk of GORD due to hormonal changes and elevated intra-abdominal pressure as the uterus expands. Hormones like progesterone relax the LES, contributing to reflux symptoms during pregnancy. Additionally, the growing fetus can exert pressure on the stomach, forcing acid into the esophagus.
In summary, GORD is caused by a combination of factors, including obesity, smoking, certain medications, dietary habits, and pregnancy. Understanding these underlying causes is essential for developing effective management strategies tailored to individual patients and addressing modifiable risk factors to alleviate symptoms and improve quality of life. (Nursing Paper Example on Gastrointestinal Disease: Gastroesophageal Reflux Disease (GORD)
Signs and Symptoms
Heartburn:
Heartburn is the hallmark symptom of Gastroesophageal Reflux Disease (GORD), characterized by a burning sensation in the chest or throat. It typically occurs after eating or when lying down and is caused by stomach acid refluxing into the esophagus. Heartburn can range from mild discomfort to severe pain and is often exacerbated by certain foods, beverages, or lying flat.
Regurgitation:
Regurgitation is the involuntary return of partially digested food or stomach contents into the mouth or throat. Individuals with GORD may experience a sour or bitter taste in their mouth as stomach acid regurgitates into the esophagus. Regurgitation can occur shortly after eating or when bending over and is often accompanied by a sensation of fluid moving up the chest.
Chest Pain:
Chest pain, also known as acid indigestion, is a common symptom of GORD that can mimic heart-related conditions such as angina or a heart attack. The pain may be sharp or burning and is typically located behind the breastbone. It may worsen when lying down or after consuming acidic or fatty foods. While chest pain in GORD is usually non-cardiac in nature, it should be evaluated by a healthcare professional to rule out serious cardiac conditions.
Difficulty Swallowing:
Some individuals with GORD may experience dysphagia, or difficulty swallowing, due to inflammation and irritation of the esophagus caused by acid reflux. Dysphagia can manifest as a sensation of food sticking in the throat or chest, discomfort or pain while swallowing, or the need to swallow repeatedly to move food down. Severe dysphagia may indicate complications such as esophageal strictures or narrowing.
Persistent Cough:
A chronic cough that persists despite treatment for other respiratory conditions may be a symptom of GORD. The reflux of stomach acid into the esophagus can irritate the throat and trigger coughing. This cough is often dry and persistent, particularly at night or after eating. While coughing is a common symptom of GORD, it can also be indicative of other respiratory or gastrointestinal disorders, necessitating proper evaluation by a healthcare provider.
In conclusion, GORD manifests through various signs and symptoms, including heartburn, regurgitation, chest pain, difficulty swallowing, and persistent cough. These symptoms can significantly impact an individual’s quality of life and may vary in severity depending on the frequency and extent of acid reflux. Recognizing these manifestations is crucial for timely diagnosis and management of GORD to alleviate discomfort and prevent complications. (Nursing Paper Example on Gastrointestinal Disease: Gastroesophageal Reflux Disease (GORD))

Etiology
Genetic Predisposition: While the exact cause of Gastroesophageal Reflux Disease (GORD) remains multifactorial, genetic predisposition plays a significant role in its development. Studies have identified a familial aggregation of GORD, suggesting a genetic component to the condition. Specific genetic variations may influence the function of the lower esophageal sphincter (LES) or alter gastric motility, predisposing individuals to reflux symptoms.
Obesity: Obesity is a well-established risk factor for GORD, with excess body weight contributing to increased intra-abdominal pressure. This pressure can weaken the LES, allowing gastric contents to reflux into the esophagus more easily. Adipose tissue also produces inflammatory cytokines and hormones that may further disrupt esophageal function and exacerbate reflux symptoms in obese individuals.
Hiatal Hernia: A hiatal hernia occurs when a portion of the stomach protrudes through the diaphragm into the chest cavity, disrupting the normal anatomy of the gastroesophageal junction. This structural abnormality can impair the function of the LES, leading to GORD symptoms. While not all individuals with hiatal hernias develop GORD, the presence of a hiatal hernia increases the risk of reflux and complications.
Smoking: Cigarette smoking is associated with an increased risk of GORD due to its effects on LES function and gastric motility. The chemicals in tobacco smoke can relax the LES, making it more prone to reflux. Smoking also reduces saliva production, which normally helps neutralize stomach acid in the esophagus. Consequently, smokers are more likely to experience severe and prolonged reflux symptoms.
Dietary Factors: Certain dietary habits and food choices can exacerbate GORD symptoms. Spicy, acidic, and fatty foods can irritate the esophagus and stimulate acid production, leading to increased reflux. Common trigger foods include citrus fruits, tomatoes, chocolate, caffeine, and alcohol. Large meals and lying down shortly after eating can also promote acid reflux by increasing intra-abdominal pressure. Identifying and avoiding trigger foods is essential for managing GORD symptoms.
Medications: Several medications are known to exacerbate GORD symptoms or weaken the LES, increasing the risk of reflux. Nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen and aspirin can irritate the esophageal lining and increase acid production, aggravating reflux symptoms. Additionally, calcium channel blockers used to treat hypertension and certain sedatives may relax the LES, facilitating acid reflux.
The etiology of Gastroesophageal Reflux Disease involves a complex interplay of genetic predisposition, obesity, hiatal hernias, smoking, dietary factors, and medications. Understanding these underlying contributors is essential for developing targeted management strategies and addressing modifiable risk factors to alleviate symptoms and improve quality of life. (Nursing Paper Example on Gastrointestinal Disease: Gastroesophageal Reflux Disease (GORD)
Pathophysiology
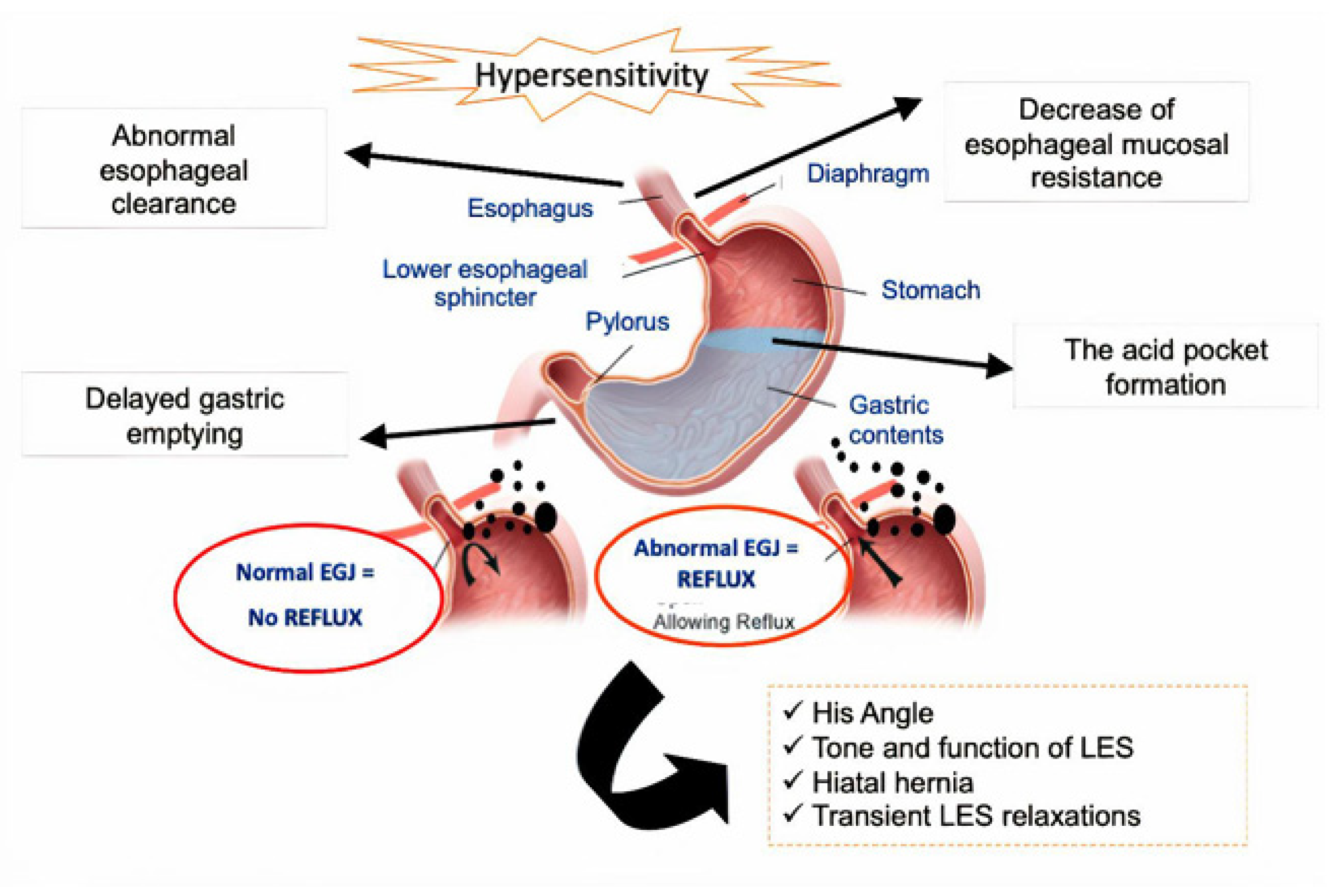
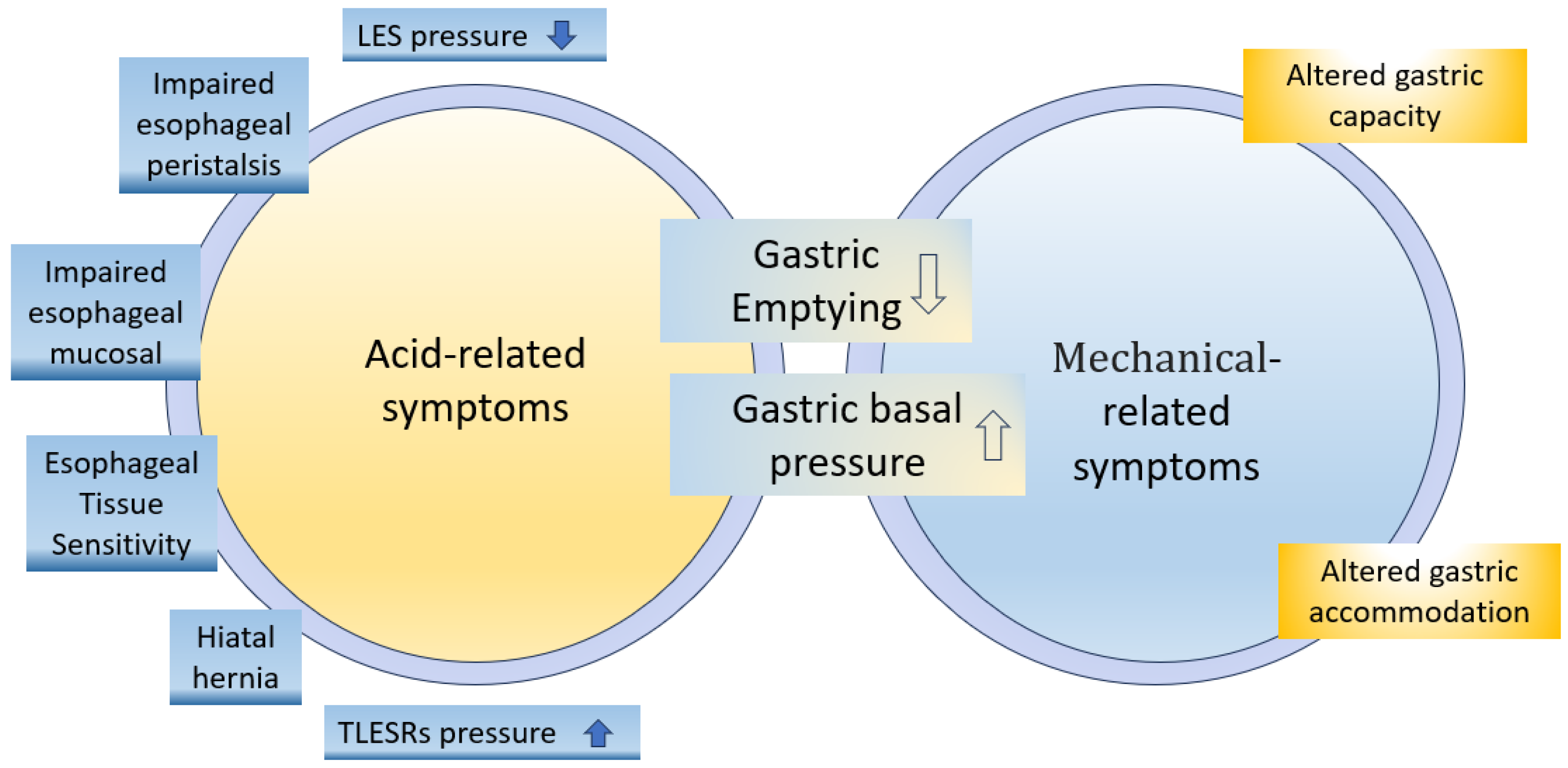
Lower Esophageal Sphincter Dysfunction: Gastroesophageal Reflux Disease (GORD) primarily involves dysfunction of the lower esophageal sphincter (LES), a muscular ring that acts as a barrier between the esophagus and the stomach. In individuals with GORD, the LES fails to close properly or relaxes inappropriately, allowing gastric contents, including stomach acid and partially digested food, to reflux into the esophagus. This malfunctioning of the LES is central to the pathophysiology of GORD and leads to the characteristic symptoms associated with the condition.
Impaired Esophageal Clearance: Another aspect of GORD’s pathophysiology involves impaired esophageal clearance mechanisms. Normally, the esophagus has efficient mechanisms, including peristalsis and salivary neutralization, to clear refluxed material back into the stomach and neutralize gastric acid. However, in individuals with GORD, these clearance mechanisms may be compromised, leading to prolonged exposure of the esophageal mucosa to acidic gastric contents. This prolonged exposure contributes to esophageal mucosal injury and inflammation, exacerbating symptoms and potentially leading to complications such as erosive esophagitis or Barrett’s esophagus.
Esophageal Mucosal Injury and Inflammation: Repeated exposure of the esophageal mucosa to gastric acid and other corrosive contents leads to mucosal injury and inflammation in individuals with GORD. The acidic nature of gastric contents irritates the esophageal epithelium, causing tissue damage and inflammation. This inflammatory response further compromises esophageal function and exacerbates symptoms such as heartburn, regurgitation, and chest pain. Over time, chronic inflammation may contribute to the development of complications such as esophageal strictures, Barrett’s esophagus, or even esophageal adenocarcinoma in severe cases.
Potential Complications: GORD can lead to various complications due to chronic esophageal mucosal injury and inflammation. These complications may include erosive esophagitis, characterized by erosions or ulcers in the esophageal mucosa, which can cause pain and bleeding. Long-term untreated GORD may also result in the development of Barrett’s esophagus, a condition characterized by changes in the esophageal lining that predispose individuals to esophageal adenocarcinoma, a type of cancer. Additionally, severe and recurrent reflux can lead to esophageal strictures, narrowing of the esophagus that can cause difficulty swallowing and food impaction.
The pathophysiology of Gastroesophageal Reflux Disease involves dysfunction of the lower esophageal sphincter, impaired esophageal clearance mechanisms, mucosal injury, and inflammation. Chronic inflammation and mucosal injury may lead to complications such as erosive esophagitis, Barrett’s esophagus, and esophageal strictures if left untreated. Understanding the underlying pathophysiological mechanisms is essential for the effective management and prevention of complications associated with GORD. (Nursing Paper Example on Gastrointestinal Disease: Gastroesophageal Reflux Disease (GORD)).
DSM-5 Diagnosis
Clinical Evaluation: Diagnosing Gastroesophageal Reflux Disease (GORD) typically involves a comprehensive clinical evaluation based on the patient’s medical history, symptom presentation, and physical examination. Healthcare providers often rely on the presence of characteristic symptoms such as heartburn, regurgitation, chest pain, and difficulty swallowing to initiate further diagnostic investigations.
Diagnostic Criteria: While the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) does not provide specific diagnostic criteria for GORD, it emphasizes the importance of assessing symptom severity and functional impairment in making a diagnosis. Healthcare providers use standardized questionnaires or symptom scales to evaluate the frequency, intensity, and impact of reflux symptoms on the patient’s daily functioning and quality of life.
Objective Measures: In addition to clinical assessment, objective measures such as upper gastrointestinal endoscopy, esophageal pH monitoring, and esophageal manometry may be employed to confirm the diagnosis of GORD and assess the extent of esophageal mucosal injury and dysfunction. Upper gastrointestinal endoscopy allows direct visualization of the esophageal mucosa and the identification of erosions, ulcers, or other pathological changes indicative of GORD. Esophageal pH monitoring measures the frequency and duration of acid reflux episodes, providing valuable information about the severity and pattern of reflux. Esophageal manometry evaluates esophageal motility and LES function, helping to identify underlying motor disorders contributing to GORD symptoms.
Differential Diagnosis: Diagnosing GORD requires differentiation from other conditions that may present with similar symptoms, such as peptic ulcer disease, gastritis, esophageal motility disorders, and cardiac conditions like angina or myocardial infarction. Healthcare providers consider the patient’s medical history, risk factors, symptom pattern, and response to initial interventions to rule out alternative diagnoses and confirm GORD.
Multidisciplinary Approach: Diagnosing GORD often involves a multidisciplinary approach, with collaboration between primary care physicians, gastroenterologists, and other healthcare professionals. This collaborative effort ensures comprehensive evaluation, appropriate diagnostic testing, and tailored management strategies to address individual patient needs and optimize outcomes.
Diagnosing Gastroesophageal Reflux Disease relies on a comprehensive clinical evaluation, standardized symptom assessment, and objective measures to confirm the diagnosis and assess the severity and impact of symptoms. While the DSM-5 does not provide specific diagnostic criteria for GORD, it underscores the importance of evaluating symptom severity and functional impairment in making a diagnosis. Differential diagnosis and a multidisciplinary approach are essential to differentiate GORD from other conditions with similar presentations and ensure optimal management and outcomes for affected individuals. (Nursing Paper Example on Gastrointestinal Disease: Gastroesophageal Reflux Disease (GORD)
Treatment Regimens
Lifestyle Modifications: Effective management of Gastroesophageal Reflux Disease (GORD) often begins with lifestyle modifications aimed at reducing reflux symptoms and improving esophageal health. Patients are advised to avoid trigger foods and beverages known to exacerbate reflux, such as spicy, acidic, and fatty foods, caffeine, alcohol, and carbonated drinks. Additionally, consuming smaller, more frequent meals and avoiding lying down or bending over shortly after eating can help reduce intra-abdominal pressure and minimize reflux episodes.
Weight Management: Obesity is a significant risk factor for GORD, and weight management is an integral component of treatment. Patients are encouraged to achieve and maintain a healthy weight through a balanced diet and regular physical activity. Weight loss can alleviate pressure on the abdomen, reduce reflux symptoms, and improve overall esophageal health.
Elevating the Head of the Bed: Elevating the head of the bed by 6 to 8 inches can help prevent acid reflux during sleep by utilizing gravity to keep stomach contents in the stomach. Patients can achieve this elevation by using bed risers or placing blocks under the bed frame’s legs. Sleeping on a wedge-shaped pillow can also provide similar benefits by elevating the upper body during sleep.
Smoking Cessation: Smoking is a modifiable risk factor for GORD, and smoking cessation is an essential aspect of treatment. Patients are encouraged to quit smoking to reduce LES relaxation, improve esophageal motility, and decrease reflux symptoms. Healthcare providers can offer support and resources to help patients quit smoking, such as counseling, nicotine replacement therapy, or prescription medications.
Medications: Pharmacological interventions are often employed to manage GORD symptoms and reduce esophageal mucosal injury. Proton pump inhibitors (PPIs), such as omeprazole, lansoprazole, and esomeprazole, are commonly prescribed to suppress gastric acid production and promote esophageal healing. H2 receptor antagonists, such as ranitidine and famotidine, can also be used to reduce acid secretion and alleviate reflux symptoms. Antacids may provide symptomatic relief by neutralizing stomach acid, although they are less effective at healing esophageal mucosal damage.
Surgical Intervention: In refractory cases or when complications arise, surgical intervention may be considered to improve LES function and prevent reflux. Fundoplication is a surgical procedure in which the upper part of the stomach is wrapped around the LES to strengthen its closure and reduce reflux. Endoscopic procedures, such as transoral incisionless fundoplication (TIF) or radiofrequency ablation (RFA), may also be performed to tighten the LES and improve reflux control. (Nursing Paper Example on Gastrointestinal Disease: Gastroesophageal Reflux Disease (GORD)
Patient Education: Patient education is essential for empowering individuals to actively participate in their GORD management and achieve optimal outcomes. Patients should be educated about the importance of adhering to lifestyle modifications, including dietary changes, weight management, and smoking cessation, to minimize reflux symptoms and prevent complications. Healthcare providers should discuss the rationale behind recommended interventions, potential side effects of medications, and expected outcomes to enhance patient understanding and adherence.
Monitoring and Follow-Up: Regular monitoring and follow-up are crucial components of GORD management to assess treatment efficacy, adjust interventions as needed, and address any emerging concerns or complications. Patients should be encouraged to report any persistent or worsening symptoms, side effects of medications, or difficulties adhering to recommended lifestyle modifications during follow-up visits.
The management of Gastroesophageal Reflux Disease involves a multifaceted approach encompassing lifestyle modifications, pharmacological interventions, surgical options, and patient education. Tailored treatment regimens should address individual patient needs and preferences while emphasizing the importance of adherence to lifestyle modifications and regular monitoring to achieve optimal symptom control and improve esophageal health.


