Nursing Paper Example on Understanding Epilepsy: Causes, Symptoms, Diagnosis, Treatment, and Patient Education
/in Assignment Help, Assignment Help Nursing, BLOG, Homework Help, Nursing Exam Help, Nursing Paper Help, Solved Nursing Essays /by Aimee GraceNursing Paper Example on Understanding Epilepsy: Causes, Symptoms, Diagnosis, Treatment, and Patient Education
Epilepsy is a neurological disorder that affects millions of people worldwide, transcending age, gender, and ethnicity. Characterized by recurrent seizures, epilepsy poses significant challenges to those affected and their families, impacting various aspects of daily life. Despite its prevalence, epilepsy remains widely misunderstood, leading to misconceptions and stigmatization. Therefore, a comprehensive understanding of epilepsy, including its causes, signs and symptoms, diagnosis, treatment regimens, and patient education, is essential for effective management and support. This paper aims to explore the multifaceted aspects of epilepsy, shedding light on its complexities while providing insights into current practices for diagnosis, treatment, and patient care. By delving into the intricacies of epilepsy, we can foster greater awareness, empathy, and support for individuals living with this condition, ultimately working towards a more inclusive and informed society. (Nursing Paper Example on Understanding Epilepsy: Causes, Symptoms, Diagnosis, Treatment, and Patient Education)
Causes
Epilepsy can arise from various factors, both intrinsic and extrinsic to the central nervous system. One significant factor contributing to epilepsy is genetic predisposition. Certain genetic mutations or abnormalities can increase the likelihood of developing epilepsy. These genetic factors may influence the structure and function of neuronal networks, predisposing individuals to abnormal electrical activity in the brain, which can lead to seizures.
Furthermore, epilepsy can result from acquired brain injuries or abnormalities. Traumatic brain injury due to accidents or sports-related injuries can disrupt neuronal pathways and lead to epileptic seizures. Similarly, stroke, which causes damage to brain tissue due to lack of blood flow, can result in epilepsy. Brain tumors, particularly those affecting regions responsible for regulating neuronal activity, can also trigger epileptic seizures.
Infections of the central nervous system, such as meningitis or encephalitis, can lead to inflammation and scarring of brain tissue, disrupting normal neuronal function and increasing the risk of epilepsy. Developmental disorders affecting brain structure, such as cortical dysplasia or neurofibromatosis, can also predispose individuals to epilepsy.
Additionally, prenatal and perinatal factors can contribute to the development of epilepsy. Conditions such as maternal drug use, infections, or complications during childbirth can affect fetal brain development, increasing the risk of epilepsy later in life.
In some cases, the cause of epilepsy remains unknown, termed idiopathic epilepsy. While the underlying cause may not be identified, idiopathic epilepsy is believed to have a genetic component, indicating a complex interplay of genetic and environmental factors in its development.
Overall, epilepsy is a heterogeneous disorder with a multifactorial etiology. Understanding the various causes of epilepsy is crucial for tailoring treatment approaches and providing appropriate support to individuals affected by this condition. (Nursing Paper Example on Understanding Epilepsy: Causes, Symptoms, Diagnosis, Treatment, and Patient Education)
Signs and Symptoms
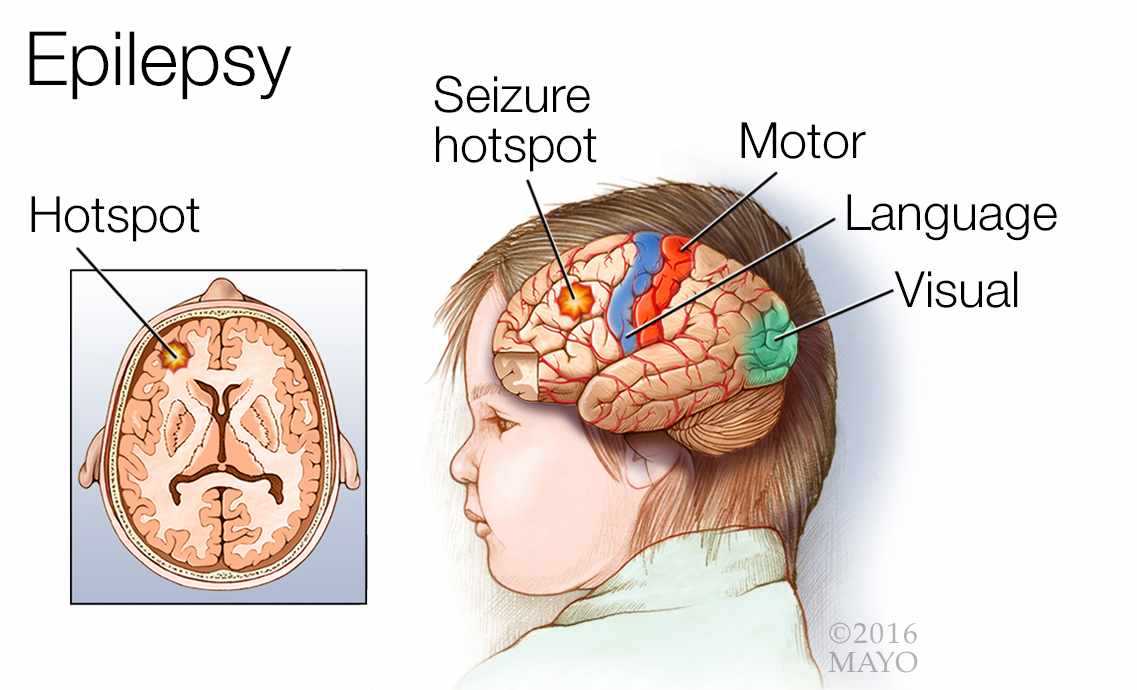
Epilepsy presents with a diverse array of signs and symptoms, often varying among individuals and across different types of seizures. The hallmark of epilepsy is the occurrence of recurrent seizures, which result from abnormal electrical activity in the brain.

Seizures can manifest in various forms, ranging from subtle changes in awareness to dramatic convulsions. Some individuals may experience focal seizures, which originate in a specific area of the brain and may be associated with sensory or motor disturbances. These seizures can cause altered consciousness, repetitive movements, or unusual sensations such as tingling or visual disturbances.
Generalized seizures involve widespread neuronal activity and can lead to loss of consciousness and uncontrolled movements. These seizures may present as tonic-clonic seizures, characterized by stiffening (tonic phase) followed by rhythmic jerking (clonic phase) of the limbs. Absence seizures, another type of generalized seizure, are brief episodes of staring or transient loss of awareness, often mistaken for daydreaming.
Other signs and symptoms of epilepsy may include auras, which are sensory disturbances or unusual sensations that precede a seizure, providing a warning sign for some individuals. Postictal symptoms, occurring after a seizure, can include confusion, fatigue, headache, or muscle soreness.
In addition to seizures, epilepsy can impact various aspects of daily life and may be associated with comorbidities such as cognitive impairments, mood disorders, or sleep disturbances. These comorbidities can further affect quality of life and require comprehensive management strategies.
It is essential for individuals with epilepsy and their caregivers to recognize the signs and symptoms of seizures, as timely intervention and appropriate management can help mitigate their impact. Furthermore, understanding the diverse manifestations of epilepsy promotes empathy and support for those affected by this condition. (Nursing Paper Example on Understanding Epilepsy: Causes, Symptoms, Diagnosis, Treatment, and Patient Education)
Etiology
Epilepsy is a complex disorder with a multifaceted etiology, involving a combination of genetic, developmental, and acquired factors. Genetic predisposition plays a significant role in the development of epilepsy, with certain genetic mutations or variations increasing susceptibility to abnormal neuronal activity in the brain. Family history of epilepsy or related neurological conditions can also contribute to an individual’s risk.
Developmental abnormalities in brain structure or function can predispose individuals to epilepsy. Conditions such as cortical dysplasia, in which the brain’s outer layer fails to develop properly, or neurofibromatosis, characterized by the growth of tumors in the nervous system, can disrupt normal neuronal networks and increase the likelihood of seizures.
Acquired factors, such as brain injury or infection, can also precipitate epilepsy. Traumatic brain injury resulting from accidents or physical trauma can cause structural damage to the brain, disrupting neuronal pathways and increasing the risk of seizures. Similarly, infections of the central nervous system, such as meningitis or encephalitis, can lead to inflammation and scarring of brain tissue, further contributing to epileptogenesis.
Prenatal and perinatal factors are also implicated in the etiology of epilepsy. Maternal factors such as drug use, infections, or complications during pregnancy can affect fetal brain development, increasing the risk of epilepsy later in life. Similarly, birth complications or perinatal injuries can impact brain function and predispose individuals to epilepsy.
In some cases, the exact cause of epilepsy remains unknown, termed idiopathic epilepsy. While the underlying mechanisms may not be fully understood, idiopathic epilepsy is believed to have a genetic component, highlighting the complex interplay of genetic and environmental factors in its etiology.
Understanding the diverse etiological factors contributing to epilepsy is essential for tailoring management strategies and providing appropriate support to individuals affected by this condition. (Nursing Paper Example on Understanding Epilepsy: Causes, Symptoms, Diagnosis, Treatment, and Patient Education)
Pathophysiology
Epilepsy is characterized by abnormal neuronal activity in the brain, leading to recurrent seizures. The pathophysiology of epilepsy involves complex interactions within neuronal networks, resulting in disruptions to normal electrical signaling and synchronization.
At the cellular level, epilepsy is associated with alterations in ion channel function and neurotransmitter release. Abnormalities in ion channels, which regulate the flow of ions across neuronal membranes, can lead to hyperexcitability or hypersynchrony of neuronal firing, predisposing individuals to seizures. Disruptions in neurotransmitter systems, such as gamma-aminobutyric acid (GABA) and glutamate, further contribute to abnormal neuronal activity in epilepsy.
Structural abnormalities in the brain can also play a role in the pathophysiology of epilepsy. Conditions such as cortical dysplasia, hippocampal sclerosis, or brain tumors can disrupt normal neuronal architecture, leading to focal areas of hyperexcitability and seizure generation.
Additionally, abnormalities in network connectivity and synchronization contribute to the generation and propagation of seizures in epilepsy. Disruptions in the balance between excitatory and inhibitory neuronal circuits can result in excessive neuronal firing and synchronization, leading to seizure activity.
The pathophysiology of epilepsy is dynamic and multifactorial, involving a complex interplay of genetic, developmental, and acquired factors. While the exact mechanisms underlying epileptogenesis remain incompletely understood, advances in neuroimaging, electrophysiology, and molecular biology have provided insights into the complex interactions within neuronal networks.
Understanding the pathophysiological mechanisms of epilepsy is crucial for developing targeted treatment strategies aimed at modulating neuronal excitability and preventing seizure generation. By elucidating the underlying mechanisms driving epileptogenesis, researchers aim to identify novel therapeutic targets and improve outcomes for individuals living with epilepsy. (Nursing Paper Example on Understanding Epilepsy: Causes, Symptoms, Diagnosis, Treatment, and Patient Education)
DSM-5 Diagnosis
The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), provides criteria for diagnosing epilepsy based on the presence of recurrent seizures and their specific characteristics. According to the DSM-5, epilepsy is classified as a neurological disorder characterized by the occurrence of at least two unprovoked seizures occurring more than 24 hours apart.
The DSM-5 outlines specific criteria for the diagnosis of epilepsy, including the documentation of seizure types, frequency, and associated features. Detailed history-taking and thorough neurological examination are essential for accurately diagnosing epilepsy and distinguishing it from other conditions that may present with seizure-like symptoms.
The DSM-5 emphasizes the importance of differentiating between various types of seizures, including focal onset seizures, generalized onset seizures, and unknown onset seizures. Detailed descriptions of seizure semiology, including motor, sensory, autonomic, and behavioral features, aid in categorizing seizures according to their origin and characteristics.
In addition to clinical evaluation, diagnostic tests such as electroencephalography (EEG), magnetic resonance imaging (MRI), and blood tests may be performed to further evaluate the underlying cause of epilepsy and assess the extent of brain involvement.
The DSM-5 also recognizes the importance of considering comorbid psychiatric conditions in individuals with epilepsy, as they may significantly impact treatment outcomes and overall quality of life. Common comorbidities include mood disorders, anxiety disorders, and cognitive impairments.
Overall, the DSM-5 provides a comprehensive framework for diagnosing epilepsy, emphasizing the importance of detailed history-taking, thorough clinical evaluation, and consideration of comorbid conditions. Accurate diagnosis and classification of epilepsy facilitate appropriate treatment selection and management, ultimately improving outcomes for individuals living with this condition. (Nursing Paper Example on Understanding Epilepsy: Causes, Symptoms, Diagnosis, Treatment, and Patient Education)
Treatment Regimens
Effective management of epilepsy requires a multifaceted approach that encompasses pharmacological interventions, lifestyle modifications, and patient education. The primary goal of treatment is to achieve seizure control while minimizing side effects and improving overall quality of life for individuals living with epilepsy.
Pharmacological Interventions: Antiepileptic medications (AEDs) are the cornerstone of epilepsy treatment. These medications work by stabilizing neuronal activity in the brain and reducing the likelihood of seizure occurrence. The selection of AEDs is tailored to the individual’s seizure type, frequency, and potential side effects. It is essential for patients to adhere to their prescribed medication regimen consistently to optimize seizure control. Regular follow-up appointments with healthcare providers are necessary to monitor treatment response and adjust medication dosages as needed.
Lifestyle Modifications: In addition to medication, lifestyle modifications can play a significant role in managing epilepsy. Strategies such as maintaining a regular sleep schedule, avoiding triggers such as alcohol or recreational drugs, managing stress through relaxation techniques, and adhering to a healthy diet may help reduce seizure frequency and improve overall well-being. Regular exercise, while promoting physical health, should be pursued cautiously, taking into account individual seizure triggers and safety precautions.
Patient Education: Patient education is paramount in empowering individuals with epilepsy to actively participate in their treatment and self-management. Key components of patient education include understanding epilepsy and its causes, recognizing seizure triggers, knowing how to respond during a seizure episode, and adhering to medication regimens. Patients should also be educated about potential side effects of AEDs and strategies for managing them effectively. Furthermore, patients and their families should receive training in administering first aid during seizures and be knowledgeable about when to seek emergency medical assistance.
Epilepsy management requires a comprehensive approach that integrates pharmacological interventions, lifestyle modifications, and patient education. By addressing seizure control, minimizing side effects, and promoting self-management strategies, individuals living with epilepsy can achieve better outcomes and enhanced quality of life. Empowering patients through education and support fosters autonomy and resilience in managing their condition, ultimately leading to improved overall well-being and functional independence. Ongoing research and advancements in treatment modalities continue to expand therapeutic options and improve outcomes for individuals affected by epilepsy. (Nursing Paper Example on Understanding Epilepsy: Causes, Symptoms, Diagnosis, Treatment, and Patient Education)
Conclusion
Epilepsy is a complex neurological disorder that requires a multifaceted approach to management. By exploring its causes, signs and symptoms, etiology, pathophysiology, DSM-5 diagnosis, treatment regimens, and patient education, we gain valuable insights into this condition. The updated discussion on treatment regimens emphasizes the importance of personalized pharmacological interventions, lifestyle modifications, and patient education in achieving optimal seizure control and enhancing quality of life for individuals with epilepsy. Furthermore, the emphasis on patient education underscores the significance of empowering patients to actively participate in their treatment and self-management. Through ongoing research and advancements in treatment modalities, there is hope for continued improvement in outcomes and support for those living with epilepsy. By fostering greater awareness, empathy, and support, we can work towards a more inclusive and informed society that better understands and supports individuals affected by epilepsy. (Nursing Paper Example on Understanding Epilepsy: Causes, Symptoms, Diagnosis, Treatment, and Patient Education)
References
https://www.ncbi.nlm.nih.gov/books/NBK430765/