The Essential Need for Self-Care in Nursing: Nurturing the Caregivers
The Essential Need for Self-Care in Nursing: Nurturing the Caregivers
Introduction
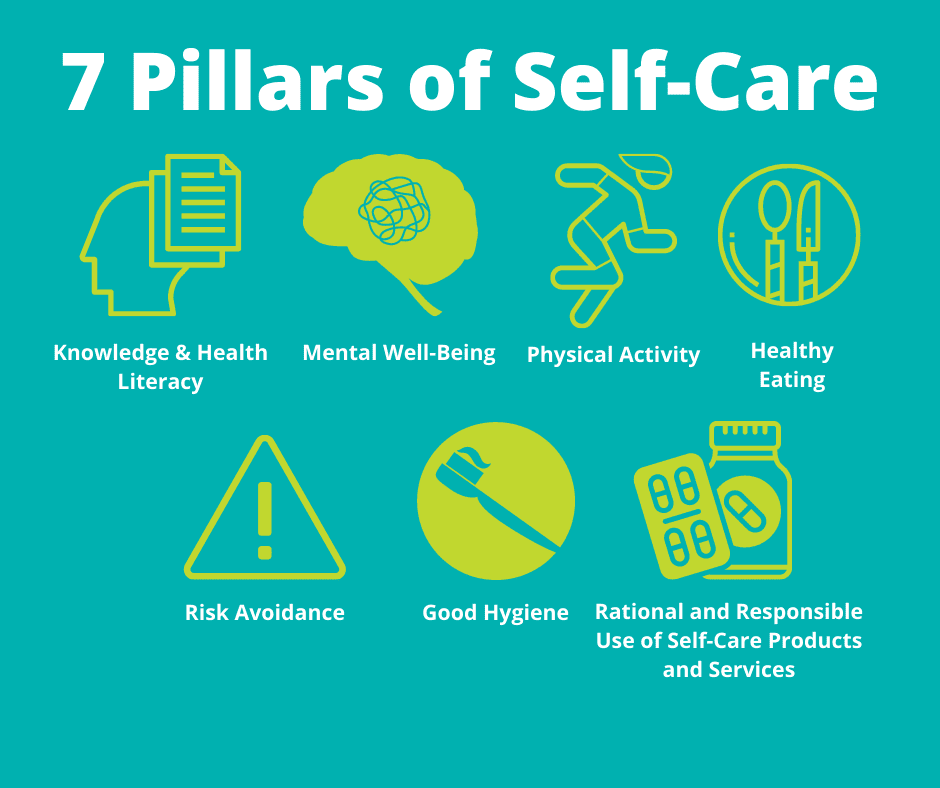
Nursing is a demanding and noble profession that requires dedication, empathy, and resilience. Nurses are the backbone of healthcare, providing essential care and support to patients. However, amidst their commitment to others, the concept of self-care often takes a back seat. The neglect of self-care in nursing can have profound consequences, affecting not only the well-being of individual nurses but also the quality of patient care. In this essay, we explore the background of self-care in nursing, various self-care theories, the consequences of neglecting self-care, the importance of prioritizing self-care in nursing, common barriers faced by nurses, and facilitators that can enhance self-care practices. Recognizing the importance of self-care is crucial for fostering a healthier and more sustainable nursing profession.

Background of Self-Care
The concept of self-care in nursing has evolved, influenced by changing perspectives on healthcare, the recognition of the interconnectedness between personal well-being and professional performance, and an increasing emphasis on holistic approaches to health. Traditionally, nursing has been framed within a paradigm of selfless dedication to patient care, often at the expense of the nurse’s own needs. This historical perspective viewed self-care as a secondary concern, with the primary focus on meeting the demands of a challenging profession.
However, as the nursing profession has matured, there has been a paradigm shift towards recognizing the vital role of self-care in sustaining a resilient and effective nursing workforce. The 20th century saw the emergence of influential nursing theorists who began to challenge the notion that prioritizing one’s well-being was incompatible with providing high-quality patient care. Dorothea Orem, a pioneer in nursing theory, introduced the Self-Care Deficit Nursing Theory, emphasizing that nurses must engage in self-care to maintain their health and, consequently, their ability to care for others effectively.
In the latter part of the 20th century and into the 21st century, societal attitudes toward health and well-being underwent significant transformations. The holistic health movement emphasized the integration of physical, mental, and emotional aspects of well-being, aligning with the core principles of nursing. Nurses began to recognize that neglecting self-care not only jeopardized their health but also had profound implications for their professional competence and the quality of patient care. The background of self-care in nursing, therefore, reflects an evolving understanding of the reciprocal relationship between the well-being of nurses and their capacity to provide compassionate and effective care. This historical context sets the stage for a contemporary approach to nursing that recognizes self-care as an essential component, fostering a more sustainable and resilient healthcare workforce.

Self-Care Theories in Nursing
Several influential theories within the field of nursing have contributed to shaping the understanding and promotion of self-care among healthcare professionals. Dorothea Orem’s Self-Care Deficit Nursing Theory is a cornerstone in this regard. Developed in the 1950s and 1960s, Orem’s theory posits that individuals, including nurses, have a fundamental need for self-care to maintain their health and well-being. The theory asserts that individuals engage in self-care activities to address self-care deficits, and nurses, by recognizing and fulfilling their own self-care needs, can enhance their ability to provide effective care to others. Orem’s model serves as a foundational framework for understanding the dynamic interplay between personal well-being and professional caregiving.
Another influential theory is the Health Promotion Model (HPM) proposed by Nola Pender. Developed in the 1980s, Pender’s HPM integrates the concept of self-care as a crucial component of health promotion. The model emphasizes the proactive engagement of individuals in behaviors that contribute to their well-being, considering factors such as individual characteristics, experiences, and environmental influences. In the context of nursing, the HPM underscores the importance of nurses actively participating in self-care practices to promote their health and, by extension, the health of the patients they serve.
Furthermore, the Theory of Human Caring, introduced by Jean Watson, emphasizes the holistic nature of nursing care. Watson’s theory posits that caring is central to nursing practice, encompassing not only the care provided to patients but also the care nurses extend to themselves. Within this framework, self-care becomes an integral part of the nurse’s commitment to holistic healing, emphasizing the interconnectedness of self-care, compassion, and effective caregiving. These self-care theories collectively contribute to a comprehensive understanding of the importance of nurses prioritizing their well-being. By recognizing and integrating these theoretical frameworks into nursing practice, healthcare professionals can foster a culture of self-care that not only benefits individual nurses but also enhances the overall quality of patient care.
Consequences of Lack of Self-Care
The failure to prioritize and engage in self-care practices among nurses can lead to a cascade of negative consequences, both for individual healthcare professionals and the broader healthcare system. One primary consequence is the prevalence of burnout. Burnout in nursing is characterized by emotional exhaustion, depersonalization, and a diminished sense of personal accomplishment. The demanding nature of the profession, coupled with the emotional intensity of caring for others, can leave nurses physically and emotionally depleted.
This burnout not only takes a toll on the mental and emotional well-being of nurses but also has tangible effects on the quality of patient care. Exhausted and overwhelmed nurses may struggle to maintain the high level of attentiveness and empathy required in their roles. As a result, patient satisfaction may decline, and the risk of medical errors or oversights increases, compromising overall patient outcomes. Furthermore, the consequences of inadequate self-care extend beyond the individual nurse to impact workforce retention. High levels of burnout and stress contribute to increased turnover rates within the nursing profession. This turnover not only leads to a loss of experienced and skilled professionals but also places additional strain on the remaining staff, perpetuating a cycle of stress and burnout.
The mental health repercussions of neglecting self-care are also significant. Nurses who consistently prioritize the needs of others over their own may experience heightened levels of stress, anxiety, and, in severe cases, depression. Mental health issues can further erode job satisfaction and overall job performance, contributing to a decline in the overall quality of healthcare delivery. In summary, the consequences of the lack of self-care in nursing are multifaceted, affecting both individual nurses and the healthcare system at large. Addressing these consequences requires a paradigm shift that recognizes self-care as a fundamental component of a nurse’s professional responsibility, essential for maintaining a resilient and effective healthcare workforce. Prioritizing self-care is not a luxury but a strategic investment in the well-being of nurses and, consequently, the quality of patient care.
Importance of Self-Care in Nursing
The importance of self-care in nursing cannot be overstated, as it plays a pivotal role in maintaining the physical, emotional, and mental well-being of healthcare professionals. Nurses are often immersed in a demanding and high-stakes environment, dedicating themselves to the care and well-being of others. In this noble pursuit, the neglect of personal self-care can have profound consequences on both individual nurses and the quality of patient care.
First and foremost, prioritizing self-care is essential for preventing burnout, a pervasive issue in the nursing profession. Burnout, characterized by emotional exhaustion, depersonalization, and a reduced sense of accomplishment, can compromise the effectiveness and compassion with which nurses approach their responsibilities. Regular engagement in self-care practices, such as exercise, mindfulness, and adequate rest, helps mitigate the impact of stressors, contributing to greater emotional resilience and job satisfaction.
Moreover, the importance of self-care extends to the preservation of mental health. The emotional demands and exposure to challenging situations can take a toll on nurses’ psychological well-being. Incorporating self-care into their routine allows nurses to process and cope with the emotional challenges inherent in their roles, reducing the risk of anxiety, depression, and compassion fatigue. A workforce that prioritizes self-care also benefits the healthcare system as a whole. Nurses who actively engage in self-care are more likely to provide high-quality, patient-centered care. Their enhanced well-being positively influences teamwork, communication, and overall job performance, contributing to a positive work environment and a culture of excellence in healthcare delivery.
In essence, the importance of self-care in nursing goes beyond individual well-being; it is integral to sustaining a resilient, compassionate, and effective healthcare workforce. Recognizing self-care as a professional responsibility not only safeguards the mental and physical health of nurses but also ensures the delivery of optimal patient care, fostering a healthcare environment that values and supports the holistic well-being of its caregivers.
Barriers to Self-Care
While the importance of self-care in nursing is widely acknowledged, numerous barriers hinder its effective integration into the daily lives of healthcare professionals. These barriers, often systemic and deeply ingrained in the culture of healthcare organizations, contribute to the ongoing challenges nurses face in prioritizing their own well-being. One significant barrier is the demanding nature of the nursing profession. Long working hours, irregular shifts, and high patient-to-nurse ratios create an environment where nurses find it challenging to carve out time for self-care. The relentless pace of healthcare delivery leaves little room for personal activities, leading to fatigue and an increased susceptibility to burnout.
Moreover, a prevailing stigma surrounding self-care in nursing exacerbates the reluctance of healthcare professionals to prioritize their well-being. There exists a cultural expectation that places the needs of patients above those of the caregivers. This mentality perpetuates the belief that taking time for oneself is selfish and conflicts with the altruistic nature of nursing. Overcoming this ingrained mindset is crucial for fostering a culture where self-care is seen as integral to sustaining a healthy and effective nursing workforce. Inadequate institutional support is another significant barrier. Many healthcare organizations lack comprehensive programs and resources dedicated to promoting self-care among their nursing staff. Insufficient access to mental health services, wellness programs, and resources for managing stress further hinders nurses from actively engaging in self-care practices.
Additionally, the organizational emphasis on productivity and meeting patient care demands often leaves little room for breaks or opportunities for self-care activities during shifts. The pressure to perform optimally within a constrained timeframe can lead to a neglect of personal needs, perpetuating a cycle of stress and burnout. Addressing these barriers requires a multifaceted approach that includes changes in organizational culture, policies, and increased awareness. Efforts to promote self-care in nursing should be supported by robust institutional initiatives, fostering an environment where nurses feel empowered to prioritize their well-being without fear of judgment or compromise to their professional commitment. Overcoming these barriers is essential for cultivating a sustainable nursing workforce capable of delivering high-quality care.
Facilitators of Self-Care in Nursing
Recognizing the barriers to self-care in nursing is crucial, but equally important is identifying and implementing facilitators that can empower healthcare professionals to prioritize their well-being. Facilitators create an enabling environment where self-care becomes not only feasible but also an integral part of the nursing culture.
- Education and Awareness: Providing education on the importance of self-care and its positive impact on both personal well-being and patient care is a foundational facilitator. Creating awareness campaigns within healthcare organizations can help dispel myths, reduce stigma, and foster a shared understanding of the significance of self-care in nursing.
- Institutional Support: Healthcare organizations play a pivotal role in facilitating self-care. Establishing policies that prioritize staff well-being, offering mental health services, and providing access to wellness programs are essential components of institutional support. When organizations actively invest in the health of their nursing staff, it creates a culture that values self-care.
- Flexible Scheduling: Implementing flexible scheduling options can empower nurses to better manage their work-life balance. Allowing for predictable and adjustable work hours, as well as incorporating rest periods into shifts, enables nurses to plan and engage in self-care activities without compromising their professional responsibilities.
- Peer Support Initiatives: Creating a supportive community within nursing teams can be a powerful facilitator. Peer support programs, where nurses can share experiences, coping strategies, and resources, build a sense of camaraderie. This not only reduces the stigma associated with self-care but also provides practical insights into integrating self-care practices into the demanding nature of the profession.
- Mental Health Resources: Offering accessible mental health resources, such as counseling services and stress management programs, provides nurses with tools to navigate the emotional challenges of their roles. Integrating mental health support into the workplace acknowledges the unique stressors inherent in nursing and demonstrates a commitment to the well-being of healthcare professionals.
- Workplace Well-Being Programs: Comprehensive workplace well-being programs that encompass physical, mental, and emotional aspects of health can serve as a structured approach to facilitating self-care. These programs may include fitness classes, mindfulness sessions, and workshops on stress reduction and resilience.
By implementing these facilitators, healthcare organizations can create an environment that encourages and supports nurses in prioritizing their self-care. The combination of awareness, organizational commitment, and peer support contributes to a cultural shift where self-care is not only accepted but actively promoted as an integral part of the nursing profession.
Conclusion
In conclusion, the essential need for self-care in nursing is paramount for the well-being of individual nurses, the sustainability of the profession, and the quality of patient care. Recognizing the historical background that has often glorified self-sacrifice, it is imperative to shift the narrative and emphasize the importance of nurturing the caregivers. Various self-care theories provide frameworks for understanding and implementing effective self-care practices. The consequences of neglecting self-care, including burnout and compromised patient outcomes, underscore the urgency of addressing this issue.
The importance of self-care in nursing cannot be overstated. It is not an indulgence but a professional responsibility that contributes to a healthier, more resilient nursing workforce. Despite the barriers that exist, proactive measures, such as education, institutional support, and peer initiatives, can facilitate the integration of self-care into the nursing culture. As we strive to create a healthcare system that prioritizes both patients and caregivers, fostering a culture of self-care in nursing is a crucial step toward building a sustainable and compassionate healthcare environment.



