( Project Evidence Synthesis and Practice Recommendation Paper (Revised))
University of Saint Augustine for Health Sciences
NUR7050: Evidence-Based Practice for Nurse Leaders
Impact of Caesarian Section of Postoperative Recovery
Postoperative recovery allows individuals to regain control over psychological, physical, habitual, and habitual functions and attain optimal psychological well-being and preoperative dependence/independence in daily activities. The maternal care, mothers recover during the postpartum period that begins after delivery and can last between six and eight weeks. Statistics indicate that 19% of maternal deaths occur during the postpartum period: between one to six days postpartum (Tikkanen et al., 2020). Although these maternal deaths are preventable, the deaths have been increasing for the last two decades. Therefore, the postpartum period for a mother is significant for short and long-term well-being.
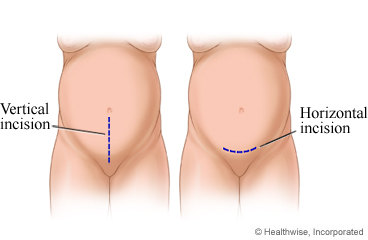
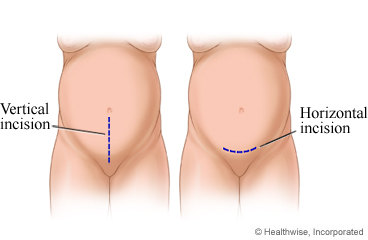
Postoperative recovery after birth depends on various aspects of pre-delivery care intending to standardize post-delivery outcomes among pregnant females. Whether a pregnant female undergoes a caesarian section or normal birth, some degree of surgical procedure influences postoperative recovery (Wilson et al., 2018). In a normal delivery, a doctor may make an incision (also known as the episiotomy) at the perineum, while a caesarian section involves a uterine or abdominal incision. These concepts justify the importance of postoperative recovery in improving maternal health outcomes, reducing postoperative hospitalization, and enhancing patient satisfaction. The paper evaluates the effect of a caesarian section on the postoperative recovery of new mothers compared to natural vaginal delivery within six weeks. ( Project Evidence Synthesis and Practice Recommendation Paper (Revised))
Significance of the Practice Problem
New Mothers face several challenges after delivery. These challenges include regaining the pre-delivery state of physical, psychological, and social well-being. The challenges are exacerbated by choice of delivery, caesarian section or normal birth, which determines the number of days before recovery following birth. The mode of delivery is a significant determinant of postpartum care among females (Chaka et al., 2019). Significantly, the rising maternal mortality during the postpartum period requires an appropriate intervention.
In the United States, more mothers die between the first and six weeks of postpartum. According to Tikkanen et al. (2020), 21% of postpartum maternal deaths occur between one and six weeks. As such, the healthcare delivery system and policymakers consistently seek ways to reverse maternal mortality. Factors such as severe bleeding, infections, and high blood pressure are commonly associated with maternal death during the first week after delivery. Besides, the USA experiences a shortage of maternity care personnel. Therefore, it is crucial to explore the impact of cesarean section on postoperative recovery to guide postpartum intervention measures.
The primary aim of every maternal healthcare team is to offer safe delivery. Caesarian section was introduced to reduce the risks for the fetus and the mother, yet mothers perceive it as an escape from labor pain. Consequently, there is a high prevalence of false supposition that a caesarian section is safer, healthier, and painless compared to natural vaginal delivery. More than 50% of women voluntarily opt for the caesarian section are the primary perseverance mode of delivery (Mazzoni et al., 2016). Studies show that first-time mothers do not have a high preference for the caesarian section. Between 6 and 8% of nulliparous women prefer a caesarian section (Mazzoni et al., 2016). The high preference of multiparous mothers for a caesarian section is attributed to safety and fear of pain.
Despite the positive health benefits, a caesarian section is associated with various health outcomes for the mother and the baby. Caesarian section affects breastfeeding initiation, low milk supply, and infant interest in breastfeeding compared to normal vaginal birth (Hobbs et al., 2016). A caesarian section is also associated with early breastfeeding cessation, and women considering a caesarian section should be guided on breastfeeding. Moreover, supportive care is crucial for lactating women undergoing a caesarian section immediately after birth and during the postpartum period.
Studies have also shown that a caesarian section affects the infant-mother relationship. According to Chen & Tan (2019), a caesarian section does not promote a healthy relationship between the infant and the mother compared to natural vaginal birth. Temmerman & Mohiddin (2021) argued that underuse or overuse of the caesarian section is associated with child survival rates on a case-by-case basis. Although a caesarian section is a lifesaving procedure in some instances, informed decisions are critical when choosing the mode of delivery for pregnant women. An informed decision is necessary to promote patient autonomy and uphold nonmaleficence.
Besides the healthcare outcomes, a caesarian section is associated with a significant economic burden compared to normal delivery. DeJoy et al. (2020) established that for women with singleton, vertex, and term pregnancies, the overall costs of caesarian procedure and newborn care are higher than natural vaginal birth by $ 5989. The economic burden of a caesarian section for consequent birth is estimated to be higher than normal vaginal birth by $4250. The increased economic burden due to a caesarian section is associated with increased length of stay and additional postpartum care requirements. These costs are born collectively by individuals, healthcare providers, and the government. ( Project Evidence Synthesis and Practice Recommendation Paper (Revised))
PICOT Question
In pregnant females (P), how does caesarian section (I) compared to natural vaginal delivery(C) affect postoperative recovery within six weeks (T)?
Population
The target population is multiparous females above 20 years of age. Studies have shown a low prevalence of C-sections among nulliparous and teenage mothers (Rydahl et al., 2019). These findings could be explained by experience with labor pain and limited knowledge of maternal health safety.
Intervention
Various factors influence the recommendation or preference for a caesarian section. Pregnant females, nulliparous or multiparous, have different preferences for mode of delivery depending on various factors related to health and attitude. The intervention, a caesarian section, involves a surgical incision at the uterine or abdominal region as a mode of delivery (Sung & Mahdy, 2022). Furthermore, the choice of C-section is influenced by the obstetric culture; culturally appropriate care (Jones et al., 2017). Different cultures have different views of a caesarian section which must be incorporated when recommending a given mode of delivery.
Comparison
Vaginal delivery involves spontaneous delivery through the vaginal opening. Spontaneous vaginal deliver delivery is the preferred mode of birth. However, studies have shown increased risks of postpartum health outcomes with maternal age (Omih & Lindow, 2016). Nulliparous females are less likely to undergo a caesarian section than multiparous females.
Outcome
Given other factors constant, the perceived outcome is an increased length of hospital stay with a caesarian section. Otherwise, a reduction in the length of hospital stay compared to natural vaginal delivery should be explained by other factors.
Timing
The postoperative recovery following will be evaluated in six weeks. The average recovery time following a C-section is documented to be between four to six weeks (Sultan & Carvalho, 2021). The proposed time is optimal for measuring the impact of caesarian delivery on postoperative recovery. ( Project Evidence Synthesis and Practice Recommendation Paper (Revised))
Search Strategy and Results
A Systematic search of electronic databases, including Academia Search Complete, MEDLINE, and CINAHL, was conducted. Search terms such as “caesarian section”, “C-section”, and “postoperative recovery” were combined into MeSH as “impact of C-section on postoperative recovery.” The inclusion criteria were articles written in English, pregnant participants followed through the postpartum period, and quantitative or systematic reviews.
A total of 478 studies were identified from the search, and ten were selected for detailed analysis.
|
|
|
|
|
|
|
|
|
| Figure 1: Flow Chart of literature search |
|
Synthesis of the Literature
Significance of the Postpartum Period
The postpartum period is significant for women as they transition from the physiological state during pregnancy to the non-pregnant state. It is a vital opportunity to improve maternal and neonatal health and well-being. It is a period of offering life-skills education, counselling mothers, educating healthy behaviors, and facilitating breastfeeding lessons for new mothers. Postpartum recovery includes supporting mothers’ mental health, recommending family planning options, and treating childbirth complications. Generally, the postpartum recovery period is significant for women’s recovery, and there is a need to improve postnatal health outcomes.
Four studies, among those selected as the body of evidence, indicated the significance of the postpartum period and how the mode of childbirth impacts postpartum recovery. According to Tikkanen et al. (2020), most maternal deaths are preventable; however, they have risen in the US compared to other high-income countries. The study attributes the high mortality rates to an overall maternity care provider shortage. In the US, women in the postpartum period have no guaranteed provider home visits or paid parental leave. The increasing rates of maternal death in the postpartum period stress the significance of the postpartum period and associated care to women’s recovery. According to Wilson et al. (2018), pre-delivery care aspects influence post-delivery outcomes. The study also stresses that any surgical procedure during birth might impact postoperative recovery. Both caesarian sections and normal deliveries might involve incisions that affect postpartum recovery. Postoperative recovery is a significant period that impacts women’s mental health and general healthcare outcomes.
The mode of delivery is a significant determinant of postpartum care among women. According to Chaka et al. (2019), the mode of delivery impacts the number of days before recovery after childbirth. Postnatal care services are fundamental elements of maternal care, affecting maternal and child health. Also, factors such as income, residence area or region, and obstetric danger signs knowledge impact access to postnatal care, reducing the odds of using postnatal care, which is significant in standardizing or optimizing the health of the mother and the child. It takes a lot for women to revert to the baseline or the non-pregnant state. Women in the postpartum period engage in breastfeeding, adapting to a new life, and maternal-neonatal bonding. Often they experience sleep deprivation. According to Sultan and Carvalho (2021), many factors, including pain, nausea, vomiting, comfort, mobilization, ability to handle the baby, loss or gain of control, hygiene, dizziness, and shivering, impact the quality of recovery. Physical function, motherhood experience, fatigue, infant health, breast health, and psychosocial support impact postpartum recovery. Conclusively, these studies indicate the importance of the postpartum period and the need to develop interventions to optimize outcomes. ( Project Evidence Synthesis and Practice Recommendation Paper (Revised))
Caesarian Sections or Normal Childbirth
The increasing rate of cesareans is also a matter of preference because more women have planned CS, even in primary childbirth. Four selected studies provided evidence of why some women prefer CS even during non-emergency situations and some factors that could influence a woman’s decision to undergo CS. Mazzoni et al. (2016) acknowledge the increasing rates of CS. The study highlights the fear of pain and safety as the most common factors influencing a preference for CS. Sex after childbirth was also expressed by most women as influencing the preference for CS. However, it is essential to note that some women preferred vaginal delivery but ended with a CS. Jones et al. (2017) found that culture influences women’s decision to undergo a CS or a vaginal childbirth. Rydahl et al. (2019) explored the association between CS and age. The study found that old age or nulliparous women aged 35-39 had double the risk for CS, and those above 40 had three times the risk. Oh and Lindow (2016) provide supportive evidence regarding the link between CS and maternal age. The study found that increasing maternal age is a risk factor for CS.( Project Evidence Synthesis and Practice Recommendation Paper (Revised))
Caesarian Sections Impact on Maternal and Natal Health
Studies have shown that the mode of child delivery impacts postoperative recovery. Women who have experienced normal childbirth tend to have shorter periods or fewer days to return to the baseline or recover to the non-pregnant state than those who have undergone a caesarian section. Among the selected studies, three provided evidence of the impact of CS on postpartum or postoperative recovery. According to Hobbs et al. (2016), the rate of CS is rising, but no significant health benefits are parallel with the rise. The study found that c-sections considerably impact breasting, including its initiation, milk supply, and child breastfeeding receptivity. The effects are more adverse compared to normal childbirths. According to Hobbs et al. (2016), the majority of females that experienced planned c-sections did not intend to breastfeed or initiate breastfeeding entirely. This number was about two times that of women with vaginal births and emergency c-sections. Also, the majority of females with emergency c-sections experienced more breastfeeding difficulties and needed more resources before and after discharge from the hospital. Women with planned c-sections were likelier to cut breastfeeding within 12 weeks postpartum. The study concludes that c-sections, whether intended or emergency, have more adverse effects on breastfeeding than vaginal births. C-sections also need more supportive care during the postpartum period.
Chen and Tan (2019) investigated whether cesarean birth can damage a woman’s health. The study acknowledges the increasing c-sections rates, which have become a social concern in many regions. The study found that c-sections significantly impact the infants’ psychological health, including their sensory perception, neuropsychiatric development, sensory integration ability, and child-mother relationships. This study is significant because it offers valuable evidence that c-sections affect maternal health and infant physical and mental health, a reason why many societies are concerned with the increasing rates. Another study by Mohiddin (2021) acknowledges women who need CS should be able to access it as a lifesaving intervention. However, whether planned or emergency, CS has short- and long-term health effects on mothers and infants. The study found CS as a significant risk factor for children’s respiratory tract infections and obesity. CS births increased the possibility of neonatal respiratory morbidity significantly. CS is also associated with a higher probability of child mortality. ( Project Evidence Synthesis and Practice Recommendation Paper (Revised))
Caesarian Sections Impact on Healthcare Cost
Generally, CS is associated with higher healthcare costs than vaginal delivery. One of the selected studies provides evidence of the significant impact of CS on healthcare costs. According to DeJoy et al. (2019), reducing CS among nulliparous women is a vital strategy towards reducing maternal morbidities and health risks to the newborn. CS is associated with high primary cesarean and newborn care costs, which is $5989 higher than vaginal births and newborn care. The cost is $4250 higher for subsequent CS and newborn care. Controlling and preventing unnecessary CS can save healthcare costs, up to $693,741 for primary and subsequent cesareans. ( Project Evidence Synthesis and Practice Recommendation Paper (Revised))
Practice Recommendation
The body of evidence provides the postpartum period as significant to a woman’s postoperative recovery. The studies also provide evidence of factors influencing the decision to undergo a CS. The body of evidence also provides supporting data on the impact of caesarian sections on maternal and infant health and healthcare costs. Based on this evidence, CS is a significant lifesaver intervention. However, the increasing rate is not parallel to health benefits, and sadly, CS is associated with adverse effects after birth, impacting postoperative recovery and postnatal care. There is a need to control CS and reduce unnecessary c-sections. Also, there is an urgency to optimize postnatal care for women who have experienced c-sections birth to address the health risks associated with the procedure. Non-clinical interventions to prevent unnecessary c-sections can be adopted. These include educating patients, their partners, and healthcare providers on prenatal care to reduce the risk of CS. Also, the intervention consists of enhanced recovery protocols after CS. If CS is anticipated, maternal comorbidities should be optimized before the operation to reduce the risk of complications such as anemia, diabetes, obesity, and hypertension and optimize maternal and natal health outcomes. The evidence is consistent, results are generalizable, studies used representative and sufficient samples, and conclusions are definitive. Based on this assessment, the recommendation is grade A or high quality. ( Project Evidence Synthesis and Practice Recommendation Paper (Revised))
Conclusion
The paper intended to investigate the impact of caesarian sections on postoperative recovery. The investigation found that the postpartum period differs for CS and vaginal births. Also, evidence indicates that CS rates are on the rise with no reciprocating health benefits. Sadly, CS is associated with adverse effects on maternal and natal health. Moreover, CS significantly adds to healthcare costs. Based on the evidence, educating women, partners, and healthcare professionals and enhancing postnatal care can help alleviate the problems associated with CS. Education can help prevent unnecessary CS and improve postnatal care to optimize postoperative recovery. ( Project Evidence Synthesis and Practice Recommendation Paper (Revised))
References
Chaka, E. E., Abdurahman, A. A., Nedjat, S., & Majdzadeh, R. (2019). Utilization and determinants of postnatal care services in Ethiopia: a systematic review and meta-analysis. Ethiopian Journal of Health Sciences, 29(1). https://doi.org/10.4314%2Fejhs.v29i1.16
Chen, H., & Tan, D. (2019). Cesarean section or natural childbirth? Cesarean birth may damage your health. Frontiers in Psychology, 10, 351. https://doi.org/10.3389/fpsyg.2019.00351
DeJoy, S. A., Bohl, M. G., Mahoney, K., & Blake, C. (2020). Estimating the financial impact of reducing primary cesareans. Journal of Midwifery & Women’s Health, 65(1), 56-63. https://doi.org/10.1111/jmwh.13010
Hobbs, A. J., Mannion, C. A., McDonald, S. W., Brockway, M., & Tough, S. C. (2016). The impact of cesarean section on breastfeeding initiation, duration, and difficulties in the first four months postpartum. BMC Pregnancy and Childbirth, 16(1), 1-9. https://doi.org/10.1186/s12884-016-0876-1
Jones, E., Lattof, S. R., & Coast, E. (2017). Interventions to provide culturally-appropriate maternity care services: factors affecting implementation. BMC Pregnancy and Childbirth, 17(1), 1-10. https://doi.org/10.1186/s12884-017-1449-7
Mazzoni, A., Althabe, F., Gutierrez, L., Gibbons, L., Liu, N. H., Bonotti, A. M., … & Belizán, J. M. (2016). Women’s preferences and mode of delivery in public and private hospitals: a prospective cohort study. BMC Pregnancy and Childbirth, 16(1), 1-8. https://doi.org/10.1186/s12884-016-0824-0
Omih, E. E., & Lindow, S. (2016). Impact of maternal age on delivery outcomes following spontaneous labor at term. Journal of Perinatal Medicine, 44(7), 773-777. https://doi.org/10.1515/jpm-2015-0128 Rydahl, E., Declercq, E., Juhl, M., & Maimburg, R. D. (2019). Cesarean section on the rise—Does advanced maternal age explain the increase? A population register-based study. PloS one, 14(1), e0210655. https://doi.org/10.1371%2Fjournal.pone.0210655
Sultan, P., & Carvalho, B. (2021). Postpartum recovery: what does it take to get back to a baseline? Current Opinion in Obstetrics and Gynecology, 33(2), 86-93. https://doi.org/10.1097/gco.0000000000000684
Sung, S., & Mahdy, H. (2022). Cesarean section. In StatPearls [Internet]. StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK546707/
Temmerman, M., & Mohiddin, A. (2021). Cesarean section: More than a maternal health issue. PLoS Medicine, 18(10), e1003792.
Tikkanen, R., Gunja, M. Z., FitzGerald, M., & Zephyrin, L. (2020). Maternal mortality and maternity care in the United States compared to 10 other developed countries. The Commonwealth Fund, 10. https://www.commonwealthfund.org/publications/issue-briefs/2020/nov/maternal-mortality-maternity-care-us-compared-10-countries
Wilson, R. D., Caughey, A. B., Wood, S. L., Macones, G. A., Wrench, I. J., Huang, J., … & Nelson, G. (2018). Guidelines for antenatal and preoperative care in cesarean delivery: enhanced recovery after surgery society recommendations (part 1). American Journal of Obstetrics and Gynecology, 219(6), 523-e1. https://doi.org/10.1016/j.ajog.2018.09.015
Table 1
Primary Quantitative Research Evidence
| Source |
Study design
JH Level of Evidence |
Population/
Sample
Age
Race/ Ethnicity
Setting/
Location
% dropout |
Intervention (IV)
Details
Action
Duration
Fidelity |
Comparison/ Control (IV)
Details
Action
Duration
Fidelity |
Outcome (DV) &Time
Intervention vs comparison
(statistical test, value, p value)
|
Grading of evidence
JH Quality Rating |
Author’s conclusions
———–
Other outcomes of interest |
Your Conclusions
Limitations |
Fit/Useful |
| DeJoy, S. A., Bohl, M. G., Mahoney, K., & Blake, C. (2020). Estimating the financial impact of reducing primary cesareans. Journal of Midwifery & Women’s Health, 65(1), 56-63. https://doi.org/10.1111/jmwh.13010 |
Quasi experimental study
Level II
|
Baystate Medical Center
All women giving birth at the facility.
N = 1747
|
ACNM’s RPC Learning Collaborative
October 1, 2016, to March 31, 2017
|
Vaginal births
Lack of RPC Collaborative participation
|
$5989 additional costs for BTSV birth
$4250 additional cost for subsequent CS
Cost saving of $693,741 after preventing 69 primary CSs and 66 subsequent CSs
|
Quality A
|
Participation in ACNM’s RPC Learning Collaborative led to considerable savings in hospital costs in the first year without affecting quality metrics |
RPC Learning Collaborative effective in cost saving and preventing CS
Model describes only inpatient |
Yes, if it also covers for outpatients |
| Hobbs, A. J., Mannion, C. A., McDonald, S. W., Brockway, M., & Tough, S. C. (2016). The impact of cesarean section on breastfeeding initiation, duration, and difficulties in the first four months postpartum. BMC Pregnancy and Childbirth, 16(1), 1-9. https://doi.org/10.1186/s12884-016-0876-1 |
Prospective cohort study
Level II
|
Calgary, Alberta
All babies within one year (2008)
N = 3021 |
Anticipatory guidance around breastfeeding
Supportive care
<25 and 34–36 weeks gestation and approximately 4 months postpartum |
Vaginal births |
Planned CS, women had not intention to breastfeed or never initiated breastfeeding (7.4 % and 4.3 % respectively) compared to vaginal births (3.4 % and 1.8 %, respectively) and emergency CS (2.7 % and 2.5 %, respectively)
Emergency CS, women had higher breastfeeding proportion (41%) and utilized more resources before (67%) and after (58%) |
Quality A |
Planned CS is linked to early breastfeeding cessation.
Anticipatory guidance and additional supportive care can help with breastfeeding struggles. |
CS has an impact on women’s breastfeeding. |
Yes |
| Mazzoni, A., Althabe, F., Gutierrez, L., Gibbons, L., Liu, N. H., Bonotti, A. M., … & Belizán, J. M. (2016). Women’s preferences and mode of delivery in public and private hospitals: a prospective cohort study. BMC Pregnancy and Childbirth, 16(1), 1-8. https://doi.org/10.1186/s12884-016-0824-0 |
Prospective cohort study
Level II
|
Two public and three private hospitals in Buenos Aires, Argentina
382 nulliparous pregnant women (183 from the private sector and 199 from the public sector)
18-35 years
Pregnancies over 32 weeks of gestation age
October 2010-September 2011 |
Assessing women’s preference about mode of delivery. Nulliparous women studied |
Other types of women. |
Only 8 and 6 % of the healthy nulliparous women in the public and private sectors, respectively, preferred CS. |
Quality A |
Healthy nulliparous women have a low preference for CS. |
Nulliparous women are less likely to consider CS than other category of women. |
Yes, if assessed for other category of women. |
| Omih, E. E., & Lindow, S. (2016). Impact of maternal age on delivery outcomes following spontaneous labor at term. Journal of Perinatal Medicine, 44(7), 773-777. https://doi.org/10.1515/jpm-2015-0128 |
Retrospective study
Level II |
N = 30,022
Five groups by their age of delivery: <19 years, 20-24 years, 25-29 years, 30-34 years and >35 years
|
Study on impact of maternal age on delivery outcome. |
N/A |
Increasing age in primiparae was linked to; augmentation of labor OR 2.05 (95% CI 1.73-2.43), second degree perineal tear 1.35 (1.12-1.61), assisted vaginal delivery 1.92 (1.53-2.41) and caesarean section 4.23 (3.19-5.12).
For or multipara; augmentation of labor OR 1.93 (1.05-3.52), perineal trauma 2.50 (1.85-3.34), assisted vaginal delivery 4.95 (91.82-13.35) and caesarean section 1.64 (1.13-2.38) |
Quality A |
Increasing age is an independent risk factor for operative delivery, and perineal trauma. |
Increasing age is associated with a high risk of CS and childbirth complications |
Yes. |
| Rydahl, E., Declercq, E., Juhl, M., & Maimburg, R. D. (2019). Cesarean section on the rise—Does advanced maternal age explain the increase? A population register-based study. PloS one, 14(1), e0210655. https://doi.org/10.1371%2Fjournal.pone.0210655 |
Population-based cohort study
Level II |
All Danish births
1998-2015
N = 1,122,964
Age < 30 (Preference)
Other categories: (30–34 years); (35–39 years), and (40 years and above) |
Study on relationship between advanced maternal age and CS. |
Controlled for demographic, anthropometric, health, and obstetric factors.
|
Positive association was found.
Comparing to the reference group.
Nulliparous women aged 35-39- years had double the risk for CS (adjusted odds ratio (AOR) 2.18, 95% confidence interval (CI) [2.11–2.26]), while for women of 40 years or over, the risk was more than tripled (AOR 3.64, 95% CI [3.41–3.90]).
For multiparous women aged 35-39-years the risk was more moderate, but still with an AOR of 1.56, 95% CI [1.53–1.60], and for those 40 years and above, the AOR was 2.02, 95% CI [1.92–2.09]. |
Quality A |
Increasing maternal age increases risk for CS.
Obstetric culture was found as a risk factor for CS. |
CS increases with age.
Design does not allow for causal interpretations of established associations |
Yes, if determined for other countries and populations. |
Legend:
CS – Caesarea section
Table 2
Evidence Summaries
| Source |
Study design
JH Level of Evidence |
Population/
Sample
Search strategy
Inclusion
Exclusion
N articles addressing your PICOT
Other descriptions
|
Intervention (IV)
Details
Action
Duration
Fidelity |
Comparison/ Control (IV)
Details
Action
Duration
Fidelity |
Outcome (DV)
& Time
Mean differences
Intervention vs comparison
Effect size
Heterogeneity
(statistical test, value, p value)
|
Grading of evidence
JH Quality Rating |
Author’s conclusions
——
Other outcomes of interest |
Your Conclusions
Limitations |
Fit/Useful |
| Chaka, E. E., Abdurahman, A. A., Nedjat, S., & Majdzadeh, R. (2019). Utilization and determinants of postnatal care services in Ethiopia: a systematic review and meta-analysis. Ethiopian Journal of Health Sciences, 29(1). https://doi.org/10.4314%2Fejhs.v29i1.16 |
Systematic Review and Meta-Analysis
Level I
|
PubMed, Scopus, Web of Science, and Embase
June 25, 2017
Studies on utilization and determinants of postnatal care.
Exclusions
Non-human studies, reviews, case reports, conference abstract, and letters, studies that did not report appropriate measures of association, non-full-text articles, duplicates
N = 9 articles
Mothers age: 15–49
|
Postnatal care utilization |
Antenatal care utilization, skilled service provider, being from urban area and delivery in health facility |
Pooled estimate for service utilization 32% (95% CI: 21%, 43%)
Determinants of postnatal care statistically significant for mothers with ability to decide (1.89; 1.25, 2.54), history of antenatal care utilization (2.55; 1.42, 3.68), received more than two antenatal care visits (1.84; 1.28, 2.40), and received the service from skilled service provider (3.16; 1.62, 4.70)
Mothers delivering in health facilities (2.13; 1.14, 3.12), had middle monthly income, richer, were from urban areas, and had knowledge of obstetric danger signs were significantly associated with an increase chance of utilizing postnatal care.
|
Quality A |
Antenatal care utilization, skilled labor provider, living in urban area, and delivering in a health facility significantly affected postnatal care utilization. |
Postnatal care is vital in postpartum delivery, and various factors, including antenatal care utilization affect its utilization. |
Useful – yes |
| Chen, H., & Tan, D. (2019). Cesarean section or natural childbirth? Cesarean birth may damage your health. Frontiers in Psychology, 10, 351. https://doi.org/10.3389/fpsyg.2019.00351 |
Systematic Review
Level II |
Medline, PubMed, EBSCO, and Psychlit
Studies on CS impact on infant psychological health, including sensory perception, sensory integration ability, neuropsychiatric development, and child-mother relationship.
Exclusions: Studies on CS impact on puerperas’ psychological health, studies wil less than 10 samples per group.
|
CS births impact on child’s psychological health. |
Vaginal births |
CS affects a child’s psychological health. |
Quality A |
CS impacts on children’s psychological health, including sensory perception, sensory integration ability, neuropsychiatric development, and child-mother relationship. |
CS is detrimental to a child’s health.
Limitation: limited grouping of children |
Useful – yes |
| Jones, E., Lattof, S. R., & Coast, E. (2017). Interventions to provide culturally-appropriate maternity care services: factors affecting implementation. BMC Pregnancy and Childbirth, 17(1), 1-10. https://doi.org/10.1186/s12884-017-1449-7 |
Systematic Review
Level II |
Ten electronic databases and two targeted websites
Studies on the effects of an intervention to offer culturally-appropriate care for ethno-linguistic or religious groups.
Exclusions: studies not published in English, Spanish, or French.
N = 15 studies
|
Interventions to offer culturally-appropriate maternity care services. |
N/A |
Interventions must consider wider economic, geographical, and social factors that impact ethnic-minority groups’ access to service and culturally appropriate care.
Understanding issues with current services and potential solution requires community participation.
Interventions should include respectful, person-centered care.
Cohesiveness is key in service provision.
|
Quality B
Small sample size and fairly definitive conclusions |
When implementing interventions to offer culturally-appropriate care, various factors should be considered to offer high-quality, respectful care which integrates community participation.
|
Culturally-appropriate care is key in maternity care services |
Useful – yes |
| Temmerman, M., & Mohiddin, A. (2021). Cesarean section: More than a maternal health issue. PLoS Medicine, 18(10), e1003792.
|
Review Article
Level III |
PLOS Medicine
Studies on association between CS and child mortality
Brazil
N = 5 articles
2012-2018
17,838,115 live births
|
Optimizing the use of CS |
Vaginal births |
CS was linked to 25% increase in child mortality in children delivered via CS in Robson groups with low expected CS frequencies.
Groups with high CS expected frequencies reported lower mortality rates, supporting the need for clinically indicated CS. |
Quality A |
Non-clinically indicated CS increase the risk of infant death.
Overuse of CS is a concern due to associated high child mortality rates.
Interventions to prevent or reduce unnecessary CS are needed urgently |
CS increase the risk of child mortality.
The rise in CS frequency is a social concern that need urgent addressing. |
Useful – yes |
| Tikkanen, R., Gunja, M. Z., FitzGerald, M., & Zephyrin, L. (2020). Maternal mortality and maternity care in the United States compared to 10 other developed countries. The Commonwealth Fund, 10. https://www.commonwealthfund.org/publications/issue-briefs/2020/nov/maternal-mortality-maternity-care-us-compared-10-countries |
Non-experimental study
Level III |
Data from CDC, Organization for Economic Co-operation and Development, and Grey literature |
Reducing maternal mortality rate |
Compared with 10 other high-income countries |
US has the highest maternal mortality rate than other high-income countries.
US has an overrepresentation of obstetrician-gynecologists.
US experiences a shortage of maternity care providers.
US does not guarantee proper access to provider home visits and paid leave compared to other high-income countries. |
Quality A |
US has a relatively low supply of maternity care providers, particularly midwives and does not offer postpartum support. |
Maternity care and postpartum support is crucial in postpartum recovery. |
Useful – yes |
Legend:
CS – Caesarea section
CDC – Centers for Disease Control and Prevention
Table 3.
Synthesis Matrix
| Main ideas |
Tikkanen et al. (2020) |
Wilson et al. (2018) |
Chaka et al. (2019) |
Carvalho (2021) |
Mazzoni et al. (2016) |
Jones et al. (2017) |
Rydahl et al. (2019) |
Oh and Lindow (2016) |
Hobbs et al. (2016) |
Chen and Tan (2019) |
Mohiddin (2021) |
DeJoy et al. (2019) |
| Significance of postpartum period |
The high mortality rates are attributed to an overall maternity care provider shortage |
Pre-delivery care aspects influence post-delivery outcomes.
Postoperative recovery is a significant period that impacts women’s mental health and general healthcare outcomes. |
The mode of delivery impacts the number of days before recovery after childbirth.
Postnatal care services are fundamental elements of maternal care, affecting maternal and child health. |
Pain, nausea, vomiting, comfort, mobilization, ability to handle the baby, loss or gain of control, hygiene, dizziness, and shivering, impact the quality of recovery.
Physical function, motherhood experience, fatigue, infant health, breast health, and psychosocial support impact postpartum recovery. |
|
|
|
|
|
|
|
|
| Factors influencing the preference for CS |
|
|
|
|
The fear of pain and safety as the most common factors influencing a preference for CS.
Sex after childbirth was also expressed by most women as influencing the preference for CS |
Culture influences women’s decision to undergo a CS or a vaginal childbirth |
Old age or nulliparous women aged 35-39 had double the risk for CS, and those above 40 had three times the risk |
Increasing maternal age is a risk factor for CS |
|
|
|
|
| Impact of CS on maternal and natal health |
|
|
|
|
|
|
|
|
C-sections considerably impact breasting, including its initiation, milk supply, and child breastfeeding receptivity. |
c-sections significantly impact the infants’ psychological health, including their sensory perception, neuropsychiatric development, sensory integration ability, and child-mother relationships |
CS as a significant risk factor for children’s respiratory tract infections and obesity |
|
| Impact on CS on healthcare costs |
|
|
|
|
|
|
|
|
|
|
|
CS is associated with higher healthcare costs than vaginal delivery |
Figure 1
Results of Search for Research
Do you need a similar assignment done for you from scratch? Order now!
Use Discount Code "Newclient" for a 15% Discount!